It’s proving very hard to move the needle. Over the last several years, the biopharmaceutical industry worldwide has intensified its focus on quality in manufacturing—but with little to show for it. Manufacturing quality levels remain well below those in other industries, such as semiconductor manufacturing and aerospace. And major recalls are still all too common. From 2010 through 2014, 11 of the top 15 biopharmaceutical companies (by revenue) received warning letters from the US Food and Drug Administration. Such problems can come at a steep price—in some cases, hundreds of millions of dollars in lost revenue, remediation costs that run in the tens of millions of dollars, and a big hit to the company’s reputation.
There are a number of reasons for the persistent quality challenges. First, the focus on quality has itself too often meant racing to put out fires when compliance issues surface, instead of addressing the root causes of quality problems. Increased investment in areas such as quality personnel or software can help in the short term, but the resulting improvements are rarely sustained and are not always commensurate with the investment. Second, when a company does implement a program aimed at delivering long-term results, it is often rolled out in a rigid, one-size-fits-all manner that ignores differences among manufacturing plants and their progress in improving quality. The result can be programs that are poorly matched to individual facilities and that miss the root causes of their quality problems. Further, such programs typically reside exclusively within the quality function and fail to address organization-wide processes that can have a major impact on quality.
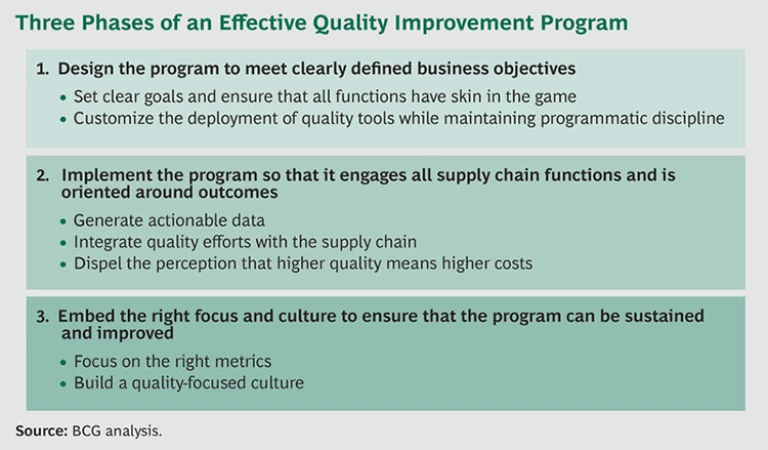
It doesn’t have to be this way. Companies can improve the effectiveness and efficiency of their quality efforts by crafting and implementing a comprehensive program that takes the entire supply chain into account, from the materials provided by key vendors to production, packaging, disposition, and distribution. To do so, they need to squarely address the factors that drive success in the three phases of
a quality improvement program:
- Designing the program to meet clearly defined business objectives, such as accelerating new-product launches, and to allow flexibility in how quality tools are deployed at the plant level.
- Implementing the program so that it engages all functions in the biopharma supply chain and is oriented around outcomes. Central to this is the tracking of actionable data so that steps can be taken to resolve problems such as high deviation rates.
- Embedding the right focus and culture so that the program can be sustained and improved. A quality-centric culture gives employees a clear understanding of how their actions affect quality and business results.
In embracing this approach, biopharmaceutical companies will be following the example of other industries in which such strategies have had powerful results.
Biopharma’s Quality Problem
In some ways it is not surprising that quality in biopharmaceutical manufacturing tends to lag that of other industries. The time line for drug development is long, and changing manufacturing processes can entail regulatory issues; as a result, many of the processes for manufacturing drugs are 10, 15, or even 20-plus years old. Industries in which product lives are shorter can revamp and improve manufacturing more frequently.
But pressure is building for biopharmaceutical companies to up their game in quality. The FDA is working with the industry to identify metrics that the agency can track across all companies and manufacturing plants—a move that will allow for greater insight into quality issues and trends.
This is happening as companies face a wave of patent expirations on blockbuster drugs, creating the need to reduce costs in order to preserve margins. While some in the industry assume that higher quality inevitably comes with higher costs, in fact the opposite is true. Certainly the investment in quality is significant: by our estimates, the biopharma industry spends about 2 to 3 percent of revenues annually, or $10 billion to $15 billion, on the quality organization. But an effective quality program is a crucial way to reduce costs, cutting the waste and other costs associated with poor quality. We estimate that moving the industry to a 3.5 sigma level from the current estimated level of 2.5 would yield significant cost savings—up to $25 billion annually—as less defective product is produced and the greater reliability of manufacturing allows companies to lower inventory levels.
Biopharmaceutical companies are launching ambitious quality improvement programs, often involving investments in new tools and technologies for tracking quality. But while some companies are successfully addressing some of the areas we have identified as crucial to a quality transformation, few are systematically addressing all of them.
The experience of companies in industries that operate at sigma levels well above those of the biopharmaceutical industry shows the power of a strategic approach to quality. A leading automaker, for example, struggled for years with quality challenges. After a number of false starts, management embarked on an ambitious quality program that addressed the critical elements within each of the three phases outlined above: it drew multiple functions into the effort, closely tracked key quality outcome metrics, and embedded a culture focused on quality. The company now boasts customer satisfaction ratings well above the industry average. We believe that biopharmaceutical companies that likewise adopt such a comprehensive strategy can expect analogous results.
Moving From Quality Laggard to Leader
In order for quality efforts to deliver maximum impact, they must involve more than just the quality organization.
Design the Program to Meet Clearly Defined Business Objectives
The first step in any major quality improvement program is to clearly spell out the objectives of the initiative and ensure that functions across the company have a stake in meeting those goals. The second step is to use a disciplined, programmatic approach that allows for the tailored deployment of centrally created tools, systems, and methodologies to individual plants.
Set clear goals and ensure that all functions have skin in the game. It is critical to define success in the right way. Quality programs often have explicit objectives linked to quality outcomes (such as a reduction in the rate of deviations in product batches), quality process targets (such as the time required to close an investigation), or quality process inputs (such as training). While those goals are important, the quality improvement effort should also be linked to broader business goals, such as increasing the speed to market of new products.
In the biopharmaceutical industry, quality programs tend to be designed and directed by the quality organization rather than by functions across the company, including manufacturing and R&D. With limited involvement from this broader group, underlying manufacturing systems and processes are not designed (or redesigned) to deliver on both the targeted quality outcomes and the company’s business goals. As a result, the manufacturing operation often has very low levels of “process robustness,” or the ability to deliver consistently high-quality product despite variations in inputs (such as operator experience). In addition, manufacturing workers typically do not own and run the critical quality processes. For example, even though most investigations are triggered by shop floor activities, responsibility for corrective and preventive action (CAPA) usually resides with the quality organization.
Establishing goals that are tied to the company’s broader business objectives helps break down this silo mentality, giving functions outside the quality organization some skin in the game. And embedding quality improvement programs across functions, such as by giving joint responsibility to manufacturing and the quality organization, will help deliver a more sustained impact over time.
Customize the deployment of quality tools while maintaining programmatic discipline. Quality improvement programs fall along a spectrum, from those that are entirely dictated by headquarters to those that are driven by the individual manufacturing plant. Although it is typically more efficient to roll out quality tools such as lean labs and standard work across the entire manufacturing network simultaneously, the top-down approach can cause plants to adopt tools that they may not need, simply because they are mandated.
Striking the right balance is critical. The overall program must be rigorous and guarantee transparent results, which a centralized approach is more likely to ensure. A decentralized strategy, however, allows managers to adopt the quality tools that best fit the standards and capabilities of the individual plant and that reflect the degree to which it is operating in a lean manner. With a flexible approach, those on the ground at the plant can determine the sequence of projects and the tools to be used.
Implement the Program So That It Engages All Functions in the Supply Chain and Is Oriented Around Outcomes
A sound plan means little if its execution is flawed. We have observed that biopharmaceutical companies often overlook a number of critical factors when it comes to delivering a quality improvement program. These include the need for reliable data and for coordination of manufacturing and quality efforts. Companies also need to dispel the perception that higher quality inevitably comes at the expense of higher costs.
Generate actionable data. It is impossible to run an effective quality improvement program without the ability to spot and fix problems. But the generation of reliable, actionable data is hardly commonplace in the biopharmaceutical industry.
Take deviations—the manufacture of intermediate or final products that do not meet specifications, or the failure to adhere to standard operating procedures. Often deviations are not tracked and analyzed in a way that can lead to effective corrective and preventive actions, such as by reactor or tank number. Or a company may analyze performance over a single quarter when tracking performance over a longer period would be needed to bring a problem to light. Similarly, companies often evaluate data for a single area within a manufacturing site when only data from multiple buildings could reveal a problematic pattern. And even where the right data is available, companies sometimes aim to quickly resolve deviations rather than trying to identify the real root cause of the problem.
The solution is to invest in personnel and software that focus on the capture of actionable input and output data that will allow for better tracking and improvement of outcomes such as deviation rates. Once that investment is made, employees in the quality organization, purchasing, production, and other key areas can conduct regular reviews of those outcomes to ensure that the right actions are taken in the future.
Integrate quality efforts with the supply chain. When the work of the quality organization—both quality control and quality assurance—is not integrated with the broader manufacturing operation and the global supply chain, problems often emerge.
Quality control operations are run independently of other functions such as production. As a result, quality control typically makes operational decisions, rolls out new IT systems, and implements programs like lean labs without integrating them with efforts undertaken elsewhere. While this arrangement can improve the efficiency of quality control itself, it can create inefficiencies in the broader supply chain. For example, a quality control lab may extend the interval between testing of product batches in order to minimize its own costs, but this may delay release times or temporarily idle manufacturing capacity further down the line. Similarly, quality control’s information management system may not be integrated into the enterprise resource planning (ERP) system used throughout the supply chain. The result: tracking of batch testing and release times is done automatically by one function and manually by others, leading to redundant work and inefficiency.
Quality assurance likewise manages critical steps in the manufacturing process, such as batch disposition—the process of determining that all required quality results, documentation, and procedures are complete before a batch of product is sent on to the next production phase or to end customers. If quality assurance fails to perform batch disposition at predictable intervals, disruption, delay, or lulls in manufacturing and shipping operations can result.
One way to integrate the quality organization into the supply chain is to segment the work of the quality control labs by customer category. For example, a biopharmaceutical company that faced cost pressures within the quality operation at one of its manufacturing plants split the work of the labs into two categories: processes required by the company’s own internal manufacturing operations and processes required by external customers. This enabled the plant to tailor investment levels on the basis of each segment’s requirements. A key benefit was that the portion of the lab focused on external manufacturing could more effectively coordinate its work according to the needs and schedules of downstream customers.
Companies can also integrate the IT systems of the quality control labs with those of manufacturing’s ERP system to strip out inefficiencies. And changing the approach to scheduling can help improve coordination between the quality organization and manufacturing. For example, coordinating the release of product batches with the schedules for manufacturing and shipping will reduce the likelihood of product shortages and the use of costly expedited shipping options. Tools such as standard work can also be a valuable element in a well-coordinated approach to scheduling.
Dispel the perception that higher quality means higher costs. Our work in manufacturing and quality has shown that improving quality does not necessarily come at the expense of higher costs. Indeed, quality operations can deploy lean methods, including standard work, to drive consistency and better outcomes while reducing costs.
In quality operations—as in most business operations—significant effort is devoted to activities that do not always add value. In quality assurance, for example, it is common to see multiple reviews by different people of the same document, and poor (or no) scheduling of the review process for the documentation that accompanies each product batch. In quality control labs, manual processes are often the norm, even when automated systems are available in the industry. This state of affairs not only fails to improve quality but also increases production lead times and lead time variability, absorbing resources and creating unnecessary redundancies.
One of the most effective tactics for eliminating such nonvalue-adding activities is to minimize the number of “small” change controls and to reduce and standardize the documentation associated with batch testing. This allows quality assurance, quality control, and manufacturing employees to focus on the things that really matter.
At one biopharmaceutical manufacturing plant, for example, management began digging into the reasons for the plant’s backlog of batch records and found that some were taking close to 100 days to close out. The review process was not only holding up the release of product batches, it was also creating inefficiencies in quality control and production. Data analysis and interviews revealed the root cause of the problem: last-minute reviews tied to product batches that for one reason or another needed to be rushed. The constant reprioritization and ad hoc scheduling of batches were slowing down the entire process and making it impossible for the quality assurance group to plan effectively.
In response, the company developed a “two lane” system for batch reviews: a standard lane and an express lane for last-minute, time-sensitive requests. This approach slashed the turnaround time for batch record reviews by more than 30 percent, while also yielding reviews that were more accurate and consistent. More important, the new system improved the connection between quality assurance and the production operation, resulting in better communication, clearer expectations on both sides, and better quality outcomes.
Embed the Right Focus and Culture So That the Program Can Be Sustained and Improved
Too often, the initial momentum of a quality program fails to be sustained. In order to maintain progress—and keep the program improving over time—it’s critical to identify the right measures of success and to build a culture that is focused on quality.
Focus on the right metrics. Companies individually—and the biopharmaceutical industry as a whole—must make a commitment to tracking progress in three categories: quality processes, quality outcomes, and business impact. By taking a balanced approach to these metrics, companies can identify which efforts are having an impact and can tailor their investments more effectively.
The FDA’s efforts to identify industry-wide quality metrics will provide momentum to this effort. But more needs to be done at the level of the individual company. While most biopharma companies do outline key metrics when they roll out a quality improvement program, too often these measures focus on inputs: statistics such as the number of certifications or the number of projects completed. While programs to build fundamental capabilities are vital to any change effort, focusing only on input metrics such as training sessions is not enough. Instead, companies should tie their initiatives to specific output measures, such as lower deviation rates, reduced waste, and improved business results.
Build a quality-focused culture. Underpinning the entire quality effort is the corporate culture. Many companies have a culture of compliance, whose primary emphasis is adherence to established rules. What is needed, however, is a true quality culture—one that goes beyond meeting standards and instead focuses on what the rules are meant to achieve.
Companies with a compliance culture will often address human performance errors by trying to influence worker behavior on the front end—by retraining, for example, or establishing new standard operating procedures. But the effectiveness of such measures can be limited. Our work in biopharmaceutical manufacturing indicates that consequences, such as awards and other types of recognition for outstanding work, are four times more effective in changing behavior than front-end measures aimed at changing how workers operate. (See The ABCs of Behavioral Change in Biopharma Manufacturing , BCG Focus, November 2013.)
Consider the case of a manufacturing plant that operated in a persistent fire-fighting mode, scrambling to address one quality challenge after another. At the root of the problem was a culture characterized by a lack of accountability and discipline and a siloed mind-set that inhibited collaboration. BCG’s extensive diagnostic, including in-depth data analysis and employee interviews, provided the foundation for a plan to fundamentally alter the plant’s culture. Among the levers: a reward for the shift that produced the largest number of defect-free batches in the previous 30 days and the posting of information throughout the plant on progress in certain critical manufacturing processes. As a result, the plant saw gains in quality and a reduction in lead time, which, in turn, boosted capacity and helped the company meet its business objectives.
A Strategy for Quality Improvement
There is no doubt that companies across the biopharmaceutical industry have taken measures to up their game in quality. But it’s time to acknowledge that current approaches are not delivering improvements quickly enough. At the heart of the problem is the fact that quality efforts are often insufficiently tied to data on outcomes, are too rigidly designed to be implemented successfully across the manufacturing network, and are isolated within the quality organization rather than integrated across the entire supply chain.
But this reality creates tremendous opportunity. Companies can drive major gains in quality programs by assessing where they stand today and redesigning their approach to be centered on results. This includes establishing the infrastructure and systems needed to track and measure progress, ensuring ownership of the effort across the organization, and building a quality-centric culture. Such an approach will amount to a redefinition and reinvigoration of the quality effort—one that requires a well-crafted strategy for moving the quality needle.