In the global debate about value-based health care , the lion’s share of attention has focused on the developed world. It makes sense. The new emphasis on value is, in large part, a response to the failure of conventional cost-control initiatives to stop or slow the rapid growth in health care costs. And the vast majority of those costs—roughly three-quarters of global expenditures on health care—are in the developed world. (See “The Case for Value-Based Health Care.”)
THE CASE FOR VALUE-BASED HEALTH CARE
In the global struggle to manage the cost of health care, both clinicians and policymakers are increasingly focusing on value. By analyzing the results achieved and resources used in well-defined patient populations (for example, diabetics or the frail elderly), health systems around the world are starting to document large variations in health outcomes as well as extensive differences in clinical practice.
Making the data available allows clinicians to identify best practices and helps to steer resources toward the clinical centers and specific clinical interventions that achieve the best results. Such efforts are facilitated by the proliferation of new systems and capabilities in health care informatics that make it possible to collect outcomes data and share it broadly with clinicians and the public. We call the delivery of improved health outcomes for defined segments of the population at the same or lower cost value-based health care.
The cornerstone of the value-based approach to care delivery is the systematic measurement of health outcomes by disease (for example, diabetes), procedure (for instance, hip replacement), or segment of the population (say, the frail elderly). The systematic collection of detailed information on health outcomes makes it possible to identify variations in outcomes across clinical sites, analyze the root causes of those variations, and codify best practices (that is, those that produce the highest-quality outcomes). Making the data and analysis transparent—in the first instance to clinicians, and eventually to the public at large—then becomes the catalyst for the definition of new standards, the dissemination of best practices across the system, the reduction of variations in outcomes, and the improvement of median health outcomes over time. (See the exhibit.)
In addition, the tracking of health outcomes and their use in continuous quality improvement make it possible to link costs to outcomes and to identify the most cost-effective types of care. This often has the positive side effect of lowering total health-care costs for some medical conditions, because unnecessary procedures are eliminated, expensive complications occur less frequently, and repeat treatments are avoided by getting it right the first time.
Another key dimension of value-based health care is the integration of clinical care for specific medical conditions and the populations of patients who suffer from them.
Integration allows providers to better coordinate care along the care-delivery pathway, take advantage of the learning curve associated with higher volumes, clarify roles, and improve accountability. It also allows payers to develop a global view of costs in the system and make informed trade-offs—for example, investing in preventive care in order to avoid high treatment costs at later points in the value chain.
Finally, once health outcomes are tracked systematically and care is integrated, a health system is in a position to develop meaningful value-based incentives on the basis of the accurate measurement of costs and the design of bundled payments appropriate to the disease or condition in question. Such incentives allow decision makers to orient competition among providers around value, so those providers that deliver high-value care are rewarded.
Since 2009, The Boston Consulting Group has conducted groundbreaking research on value-based health care, including on the impact of disease registries, on the best way to define health outcomes, on the challenge of eliminating unnecessary practice variation across providers, and on the potential of managed care to improve health outcomes.
BCG is a cofounder of the independent nonprofit International Consortium for Health Outcomes Measurement (ICHOM) and works with provider organizations, payers, and pharmaceutical and medical technology companies to help them design and implement value-based approaches to care delivery.
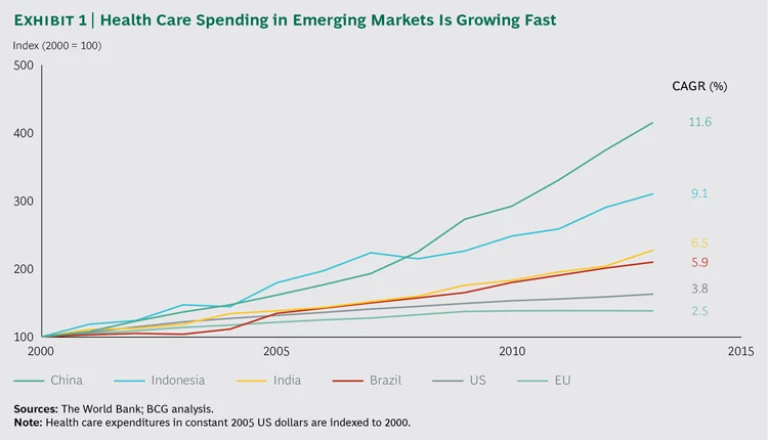
And yet, we believe that some of the biggest opportunities for value-based health care today are to be found not in advanced economies but in emerging markets. There are powerful incentives for emerging-market providers and policymakers to organize their health systems around maximizing health care value for their populations. Although these markets represent only about 25% of health care expenditures worldwide, their expenditures are growing at a much faster rate than those in the developed world. Since 2000, for example, China’s spending on health care as a percentage of GDP grew almost five times as fast as that of the EU and more than three times as fast as that of the US. (See Exhibit 1.)
Even though the GDP of emerging markets is also growing rapidly, allowing these societies to afford more health care than in the past, many of these countries do not have—and may never have—the resources to replicate the high-cost model of care delivery found in many developed countries. For example, we calculate that it would cost Nigeria $51 billion—which represents 20% of its 2012 GDP and 10 times its 2012 public health budget—simply to bring its number of physicians up to the median number in the OECD countries. And, given Nigeria’s current training infrastructure, such an expansion would take 300 years. The enormous difficulty of replicating the developed world’s care delivery model is another strong incentive for emerging markets to think differently and embrace value-based health care.
It should therefore be no surprise that some of the most interesting experiments in value-driven care delivery can be found in the developing world. To cite just one example, India’s Aravind Eye Care System is a global leader in tracking health outcomes for cataract surgery and in creating innovative care-delivery models that bring high-quality low-cost cataract surgery to India’s masses.
But before emerging markets can move beyond a few innovative providers to establish national systems for value-based health care, payers, providers, and policymakers will need to address a fundamental challenge: systematically collecting and analyzing comprehensive health outcomes data. By tracking health outcomes for the various population groups and medical conditions that represent the biggest needs in a country’s health system, stakeholders can determine the impact of investments in health care and identify innovations in care delivery that improve outcomes at the same or lower cost as previous approaches. And yet, the vast majority of emerging markets lack the necessary infrastructure—including IT systems, disease registries, and integrated health systems—typically used to collect and effectively exploit outcomes data.
The lack of an infrastructure may appear to be an insurmountable obstacle. On the contrary; we believe it represents a major opportunity. Because emerging markets are not burdened by legacy systems and the massive complexity of integrating separate data sets, they are in a position to leapfrog existing technologies and approaches. In particular, they can leverage the widespread penetration of mobile communications networks to introduce innovative approaches to connectivity and data collection and scale them up rapidly. The analogy is to what has already happened in many emerging markets in areas such as mobile telecommunications and mobile financial services. Entrepreneurs have developed entirely new infrastructures and services from scratch, bypassing the creation of traditional landline networks and physical networks of bank branches.
In the pages that follow, we first describe the leapfrogging concept in more detail. Then, to provide a concrete illustration of what it could mean for value-based health care, we introduce a BCG-designed prototype for a cloud-based mobile solution called “Our Health Journey,” which would allow patients in an emerging market to track their health outcomes using smartphones. We conclude with six principles for jump-starting value-based health care in emerging markets.
The Leapfrogging Opportunity
The concept of leapfrogging was first developed in the field of industrial organization to describe how new competitors in an industry can use radical innovations to surpass established dominant players. Over time, the idea has been expanded and applied to cities, regions, and entire countries.
For example, the World Economic Forum recently defined leapfrogging as a way for less developed economies to use innovation “
There are numerous examples of emerging markets using this leapfrogging strategy in areas unrelated to health care. The classic example is mobile financial services. In Africa, for instance, most people have extremely limited access to banking services owing to their low incomes and the absence of well-developed branch networks. And yet, millions of people in Africa today use mobile phones to transfer money, pay bills (such as insurance premiums and prepayments for electricity), and make other types of transactions. Indeed, Africans are among the world’s most enthusiastic early adopters of mobile financial services. By 2012, some 98 million people on the continent had registered mobile-financial-services accounts—the highest number in any region in the world. (See Africa Blazes a Trail in Mobile Money: Time for Banks and Mobile Operators to Devise Strategies , BCG report, February 2015.)
What is especially significant about this development is that mobile financial services are not only an add-on for people who already use banks but also a new offering, made possible by the creation of a new infrastructure, for people who have never used financial services before. For example, the M-Pesa mobile money-transfer service, an initiative of the Kenyan mobile network operator Safaricom (partially owned by Vodafone), has a network of thousands of agents who, upon receipt of a verified mobile text message, are authorized to issue cash to people in Nairobi and the Kenyan countryside, functioning much like traditional banks’ ATMs for people in the developed world. M-Pesa has steadily expanded beyond money transfers and now offers essential banking services, such as accepting cash deposits at registered retailers and enabling bill payment—even providing microinsurance. M-Pesa has also expanded its footprint beyond Kenya. By 2014, M-Pesa served 19 million people in six African countries, as well as in Afghanistan, Fiji, India, and Romania.
At first glance, it may seem as if health care, a highly personal service, is intrinsically different from financial services. After all, money is fundamentally information and, as a result, is increasingly amenable to digitization. When an individual is sick and anxious, by contrast, he or she seeks a face-to-face interaction and physical contact with a caregiver. Issues of personal and professional trust loom large.
However, more and more aspects of health care are becoming information based and are therefore able to be digitized. For example, health systems are using genetic information to create more accurate risk profiles for certain categories of patients and analyzing health outcomes data to develop insights about which treatments are effective and which are not. Digitizing information about lifestyle diseases has also created new linkages between information and personal motivation that have put changing patient behavior at the center of effective treatment. The more that digital information becomes critical to care, the more digital technologies have the potential to transform how care is organized and delivered—and the more emerging-market health systems have the potential to leapfrog previous approaches and models.
Seen from this perspective, the fact that health systems in emerging markets often lack a robust hospital network, a conventionally trained health care workforce, or a legacy IT infrastructure is not so much an obstacle as a potential advantage. The very absence of legacy systems allows these countries to start with a clean slate and invest in innovative approaches designed to maximize health outcomes at the lowest possible cost.
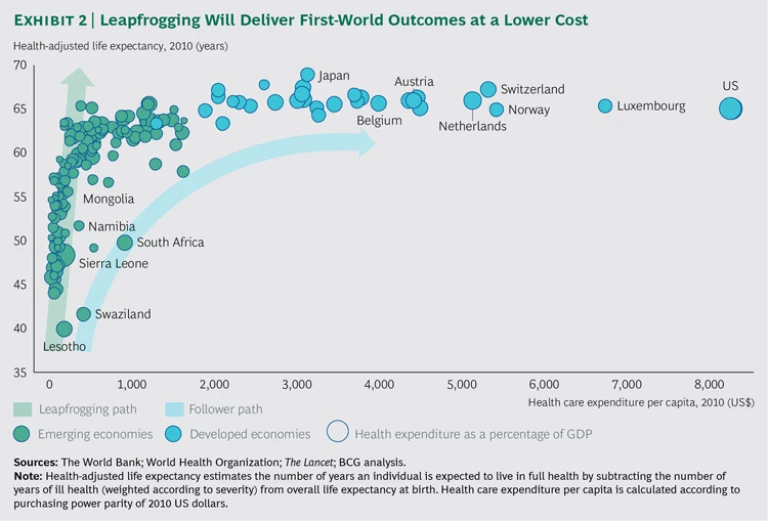
To illustrate the leapfrogging opportunity, we plotted health care expenditure per capita against health-adjusted life expectancy for 158 developed countries and emerging markets. (See Exhibit 2.) The US spends the most per capita on health care, and although it does not have the highest level of life expectancy (Japan holds that achievement and at a considerably lower cost per capita), the US and other developed countries are near the top. Meanwhile, many emerging markets, such as Lesotho or Swaziland, spend considerably less, and their levels of life expectancy are among the lowest.
By simply following the pattern of the developed countries, emerging markets will invest more money per capita to boost their average rate of health-adjusted life expectancy. However, if they pursue the leapfrogging path, they will be able to deliver higher rates of life expectancy at significantly lower cost. When it comes to value-based health care, leapfrogging is only beginning to get off the ground in emerging markets’ health systems. In some countries, pioneering provider organizations are taking the lead. In India, for example, the Aravind Eye Care System is a network of hospitals dedicated to providing low-cost, high-quality cataract surgery. It offers broad access to care, performing nearly a quarter of its surgeries for free and subsidizing roughly another quarter.
What’s more, Aravind has combined close attention to outcomes tracking with an integrated approach to care delivery. That approach is characterized by two factors. First, high volumes (the network performs more than 400,000 surgeries per year) allow surgeons to move quickly up the best-practice learning curve. Second, the existence of standardized procedures that are followed by all surgeons makes possible the rapid dissemination of the latest innovations in clinical practice. The result is first-world health outcomes at a cost per surgery that is approximately one-tenth of the cost in the US. Although Aravind’s lower cost is partially due to the relatively low salaries of cataract surgeons in India, it is primarily due to
Another Indian example is the specialty hospital chain Fortis Healthcare. In 2012, Fortis began systematically tracking its health outcomes for coronary artery disease (CAD) against global benchmarks. Today, Fortis has CAD outcomes that compare favorably with those of leading providers in the developed world.
Other initiatives are using mobile technologies as innovatively as providers of mobile financial services do. For example, the cloud-based Magpi system, developed in Kenya, allows for the mobile collection of health and other data by means of text messaging or smartphone apps. Magpi was developed by specialists in global health, disaster response, technology, and international development. Health care providers can fill out surveys on their smartphones or collect patient data by having patients fill out surveys on their traditional mobile phones and text the results back. Unicef and the Kenyan Ministry of Public Health and Sanitation have used Magpi to monitor childhood vaccination campaigns; and the World Health Organization has used the system as part of the Global Polio Eradication Initiative to monitor and improve vaccination efforts.
Meanwhile, Safaricom, building on its success with M-Pesa, has launched a new venture, in collaboration with the Dutch PharmAccess Foundation, known as M-Tiba, a mobile health wallet. It administers health care payments among patients, payers, and providers, effectively tracking and monitoring the use of funds.
With the development of new software platforms such as Apple’s recently announced CareKit, which is designed to help developers build e-health applications for the iPhone and the Apple Watch, it is likely that similar applications will proliferate in the years ahead.
Making Leapfrogging Real
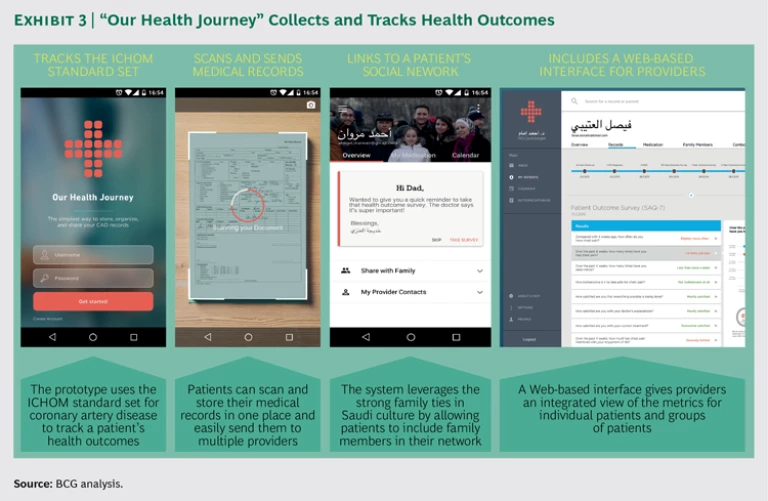
To provide a concrete illustration of how new technologies can facilitate value-based health care in emerging markets, BCG Digital Ventures, a BCG subsidiary that designs and develops digital businesses, recently developed a prototype for a mobile application that allows patients to collect and track their health outcomes data using smartphones. To emphasize that tracking health outcomes is a collective effort, requiring collaboration among providers and patients, we call the prototype “Our Health Journey.”
The cornerstone of value-based health care is the systematic measurement of health outcomes. One of the most important recent innovations in the field has been the development of comprehensive global standards by the nonprofit International Consortium of Health Outcomes Measurement. ICHOM’s mission is to convene leading physicians and patient groups from around the world to develop a consensus around the minimum set of outcomes that should be tracked for a given condition or disease. So far, ICHOM has developed 13 standard outcome sets for conditions such as stroke, hip and knee osteoarthritis, macular degeneration, and lung cancer. In 2016, the consortium plans to launch an additional 8. By 2017, the organization plans to have developed standard sets covering more than 50% of the global disease burden.
For illustrative purposes, we chose to focus the prototype on the ICHOM standard outcome set for CAD, which is widely prevalent in emerging markets. It is the top cause of mortality among noncommunicable diseases in countries such as India, Nigeria, and Saudi Arabia (accounting for 1.2 million, 130,000, and 28,000 deaths per year, respectively). The ICHOM CAD standards are also an especially well-developed set of health outcome metrics that include both clinical measures and detailed metrics for patient-reported health status.
To address the obstacles associated with collecting this data in an emerging market, we focused on Saudi Arabia as our demonstration market. The Saudi population is aging (25% will be over the age of 60 by 2050) and has a highly sedentary lifestyle—factors that are likely to make CAD an increasingly serious (and expensive) health issue in years to come. What’s more, the Saudi health system is relatively typical of the problems that emerging markets face when it comes to collecting and analyzing health outcomes data. Our analysis of the CAD treatment pathway in Saudi Arabia identified three major obstacles to the collection and analysis of the ICHOM standard outcome metrics:
- Fragmented Clinical Care. The Saudi health system is highly fragmented. Patients tend to take appointments at government hospitals as they become available. As a result, their medical records are distributed across many providers, making it difficult for any individual clinician to acquire a full picture of a patient’s medical history or health needs.
- Handwritten Records. The majority of patient records remain on paper; electronic medical records (EMRs) are uncommon in the Saudi system. According to the Saudi health ministry, only about a third of hospitals and a mere 5% of primary care centers have EMRs, which contributes to data fragmentation.
- Incomplete Clinical Data. Cardiologists typically don’t collect data on many of the outcome metrics that ICHOM has identified as critical. Patients rarely report back on their health status in the months and years after heart surgery. And the Saudi system lacks disease registries or other centralized outcomes databases that would allow the health system to examine variations in health outcomes across providers and understand what causes those variations.
To address these challenges, Our Health Journey leverages the relative absence of IT infrastructure in Saudi Arabia and the relatively high level of smartphone penetration to create a cost-effective bottom-up infrastructure for the collection of CAD-related outcomes data. (Nearly 80% of the Saudi population uses smartphones; there are currently 179 cell phone subscriptions per 100 people.)
The primary feature of Our Health Journey is a cloud-based integrated medical record that patients can complete using their smartphone. (See Exhibit 3.)
By giving patients a simple way to organize and share their medical data with providers, the app would empower patients to collaborate with their providers in order to collect and track a wide variety of outcome metrics in the ICHOM CAD standard set. And by giving providers a way to access the complete medical records of their patients, the app would empower providers to deliver more integrated care. The app would include the following functionality:
- Patients would use their smartphone’s camera to digitally scan and store their paper medical records, much as a mobile banking application allows users to electronically deposit paper checks.
- The system would identify gaps in patients’ clinical data and inform clinicians so that they can collect the necessary ICHOM data.
- The app would prompt patients to input key patient-reported metrics at appropriate intervals in the months and years after treatment.
- The app would leverage the strong familial bonds in Saudi society by making it easy for patients to designate specific family members as part of their network so that relatives can encourage and prompt patients to input data or report any missing patient-entered data.
- The system would let providers access a Web-based interface to have an integrated view of the outcome metrics for an individual patient or for groups of patients and to enable benchmarking with peer organizations.
- The system would share risk-adjusted data anonymously with the Saudi health authority so that it could analyze population-wide health outcomes data as well as compare the performance of different providers against established benchmarks.
Our Health Journey illustrates what could be possible if national health ministries, as well as large payers and leading providers, were to adopt the leapfrogging approach in a systematic fashion. Such an app could easily track a variety of ICHOM standard outcome sets and be integrated into the emerging global benchmarks for the comparison and analysis of health outcomes worldwide.
Six Principles to Jump-Start Outcomes Measurement
As emerging markets pursue innovations such as Our Health Journey, national health ministries will have a central role to play in orchestrating national systems for value-based health care. Public health authorities need to set standards for tracking health outcomes, design incentives to drive improvement, and establish a legal framework for handling confidential patient data that not only protects individual patient confidentiality but also makes anonymized data available for comparison and identification of best practices. Health ministries also need to coordinate the ecosystems of private-public partnerships that the World Economic Forum has
We have identified six principles to help national health authorities get started on this journey:
- Adapt metrics to resources. The ICHOM global standard outcome sets are designed to be minimal but sufficient criteria for assessing the quality of care. But that doesn’t mean a health system should wait until it has all the resources in place to track each of the health outcomes in a given set. A lot of value can be created by tracking a restricted set of outcomes. For example, Aravind Eye Care Systems was a lead player in the global ICHOM team that developed the standard set of outcomes to track for cataract surgery. But getting Aravind’s many uneducated and extremely poor patients to supply the patient-reported outcome measures (PROMs) in the standard set proved extremely difficult. So, for the time being, Aravind has decided not to use the PROMs in the ICHOM standard set but rather to develop a limited set of metrics more suited to the environment in which it operates.
- Leverage leapfrogging technology. A standalone system, such as the prototype Our Health Journey, is only one approach. It may also be possible to piggyback on existing applications that aren’t intended to measure health outcomes—much as M-Tiba does in the area of health spending.
- Integrate data collection along the care pathway. Collecting health outcomes data should be an integral part of every patient interaction along the care pathway. Aravind, for example, takes advantage of the routine follow-up visit 30 days after surgery to track postsurgical complications.
- Free up physician time through task shifting. Physicians are the scarce resource in most emerging-market health systems. Free up their time by leveraging other providers and patients to collect outcomes data. Aravind’s use of nurses and data entry operators, for instance, helps free up its surgeons to focus on performing a high volume of surgeries.
- Create transparency for all stakeholders. Information is power. The more stakeholders who have access to outcomes data, the more likely the data will spur changes in clinical practice or patient behavior that will improve health care value. Fortis Healthcare makes its CAD outcomes data public on the company website and updates it every six months.
- Implement practice-improvement routines. Simply sharing the data isn’t enough. To improve clinical practice, clinicians need to “interrogate” the data, figure out what it means, and consider the implications for how they deliver care. Aravind has weekly team meetings to analyze outcomes data, identify areas for improvement, and disseminate best practices.
Leapfrogging into the Future
Emerging markets have the opportunity to take a major step forward in the development of new systems for collecting and tracking health outcomes as well as alternative approaches to diagnostics, care delivery, and health monitoring—and, thus, to provide better health outcomes at lower cost. As emerging markets take this step, they may find that applications such as Our Health Journey, Aravind’s approach to cataract surgery, or Fortis Healthcare’s method for systematically benchmarking its outcomes in CAD may be extremely relevant to the circumstances of hospitals and health systems far beyond their countries and populations. (See “An Insider’s Guide to the Transformation of Health Care,” BCG article, December 2015.) The innovations in value-based health care developed in emerging markets may eventually find their way to the developed world as well.
The research described in this publication was sponsored by BCG’s Health Care practice. The authors would like to thank the following for their contributions to the research: Priyanka Aggarwal, Marc Chipot, Jennifer Clawson, Jens Deerberg-Wittram, Mark Khayat, Jan Willem Kuenen, and Gabriel Osterdahl at BCG; Mike Andersen, Jacob Perten, and Yazan Tabaza at BCG Digital Ventures; and Christina Akerman at ICHOM. They would also like to thank Robert Howard for his assistance in the conceptualization and writing of this report and Katherine Andrews, Gary Callahan, Kim Friedman, Abby Garland, Trudy Neuhaus, Sharon Slodki, and Sara Strassenreiter for their contributions to the editing, design, and production.