Many in the global health community are increasingly concerned at how little progress has been made toward the UN’s health-related Sustainable Development Goals (SDGs). Tremendous gaps remain in reaching these goals by 2030. For example, mortality of children under the age of five is projected to improve 41% worldwide by 2030, but an additional 31% will still be required to hit the SDGs, almost entirely in sub-Saharan Africa. Similarly, maternal mortality is projected to improve 32% by 2030, but an additional 29% is required to reach the goals, again mainly in sub-Saharan Africa.
The global community has achieved admirable progress in addressing global health and development challenges in recent decades. Between 2000 and 2015—the Millennium Development Goal (MDG) era—the global under-five mortality rate decreased by 58%, maternal mortality fell by 45%, and new HIV infections dropped by 40%. However, the successes of the MDGs in health were largely due to significant funding increases, focused vertical programming to combat HIV, malaria, and vaccine-preventable diseases, and an emphasis on addressing health needs in relatively easy-to-reach locations. To achieve the health SDGs, we can’t rely on this formula: a new approach is urgently needed.
The remaining challenges in global health are largely system dependent and disproportionately associated with populations that are difficult to reach.
We have identified six high-impact, no-regrets moves that we believe can help get the global community and low- and middle-income countries (LMICs) back on track to meet their ambitious 2030 global health goals.
1. Embrace “Precision Global Health”
Many global health interventions are not managed as efficiently and effectively as they could be. For example, medical supplies may be distributed widely and indiscriminately within and across countries, creating a surplus in some regions and gaps in others. Similarly, health facilities could be located more strategically in order to better serve local and regional populations. But with the rise of data and advanced analytics, precision global health can ensure that interventions and health facilities are focused on areas with the highest burden and are targeted to reach those most in need.
Global health organizations and low-income countries will need to be more strategic than ever before, doubling and in some cases quadrupling the effectiveness of spending on health.
What precision global health looks like will vary across disease areas and geographies. The examples below illustrate three distinct and evolving applications of the approach:
- Polio. Because polio is approaching eradication around the world, precision global health techniques are being executed in a highly focused manner. In the few pockets where the disease still exists, health workers conduct door-to-door campaigns to optimize vaccination targeting, in some instances relying on simple paper maps of individual neighborhoods and in others using more sophisticated techniques such as satellite imagery and geospatial mapping. In the final stages of polio elimination, when the disease has been almost entirely eradicated, precision global health can be targeted almost at the individual level.
-
Malaria. For the past 20 years, efforts to combat malaria have not generally been conducted with a high degree of precision. For example, mosquito nets have often been distributed uniformly across regions despite massive differences in incidence. As countries move closer to elimination and resources become increasingly constrained, nets (and other prophylactic and treatment products) have begun to be targeted more deliberately to those areas where malaria is most prevalent and where supplies are lacking.
For example, Tanzania’s National Malaria Control Programme now has prevention and intervention packages for different sub-regions tailored to five levels of risk. Similarly, Mali has begun to allocate resources for indoor residual insecticide spraying to districts with the highest burden and greatest potential impact. Precision health for malaria is currently operating at a subnational or district level, but in the years ahead, aided by active case detection, may increasingly be focused on hotspots.
- Zika. Over time, precision global health interventions will become proactive rather than reactive. For example, to more efficiently prevent and address outbreaks of mosquito-borne diseases like Zika and Dengue, public-health entities can use health, weather, and other data, in combination with advanced analytics, to identify areas at the highest risk for an outbreak and then execute targeted prevention efforts accordingly. In several Brazilian states and cities, health authorities have piloted AI technologies that aggregate diverse data (such as health data, historical weather patterns, and city maps) in order to identify specific high-risk neighborhoods. This has allowed them to apply precisely targeted vector control tools, such as spraying in specific neighborhoods or eliminating standing water on the roofs of apartment buildings identified as high risk. Other countries struggling with mosquito-borne illnesses have likewise begun to explore proactive precision health techniques.
While some of these techniques require a level of data and advanced analytics beyond the reach of some LMICs, others require only the aggregation of available health data and common-sense allocation of resources across countries, districts, and other smaller localities. In addition, we believe that the data and advanced analytics tools that enable precision health will become increasingly accessible even for low-resource countries in the next several years.
2. Improve Performance Management
Given the wide variability in health outcomes and lack of consistent accountability, there is a critical need to transform performance management across public-health sectors around the world. A strong performance management system allows users to aggregate and analyze key metrics on health care operations, delivery, and outcomes in order to make data-driven decisions. We have found that efforts to improve performance management in the health systems of LMICs can increase efficiency by at least 20% to 30%. When performance management data is shared publicly, facilities and clinicians have the opportunity to identify areas where they can improve the quality of care—and they can be held accountable for their performance.
Two programs, one in India and one in Kenya, illustrate the powerful effect that performance management programs can have on health systems in low-resource contexts.
The primary-care system in Rajasthan, India, a state with approximately 80 million residents, was underperforming. In 2018, as part of a performance management program called Misaal, the Rajasthan state government, in collaboration with BCG, launched a monthly district ranking. The ranking incorporated 39 metrics that covered all major diseases and practice areas, including maternal and child health, communicable diseases, and chronic conditions (like diabetes and hypertension). In order to ensure widespread impact, the rankings were made public and newspapers published articles on which districts were doing well and which were lagging. In addition, a tiered ranking process provided all districts with an opportunity to demonstrate (and celebrate) intermediate milestones. The program delivered strong results in a short period of time. For example, in less than a year, full immunization rates improved by 17% and the diabetes diagnosis rate improved by 142%. (See Exhibit 1.)
Performance management tools also had a powerful impact in Kenya, where the Global Fund—in collaboration with the health ministries of Senegal, Kenya, and Uganda—reviewed numerous health facilities to pinpoint why some were performing better than others. The BCG team involved in this effort found that top-performing health facilities in Kenya used a variety of performance management techniques to retain staff, including performance-based incentives and timely payment of salaries. The review also found that facilities with better performance management systems generally scored higher on patient satisfaction, achieved more cost efficiencies, and often (but not always) had better health outcomes, including better case detection rates and patient adherence.
These examples demonstrate how well-executed performance management initiatives in LMICs can lead to concrete improvements in health care delivery—and we believe performance management has exciting potential to improve health care in many more low-income countries.
3. Harness the Private Sector
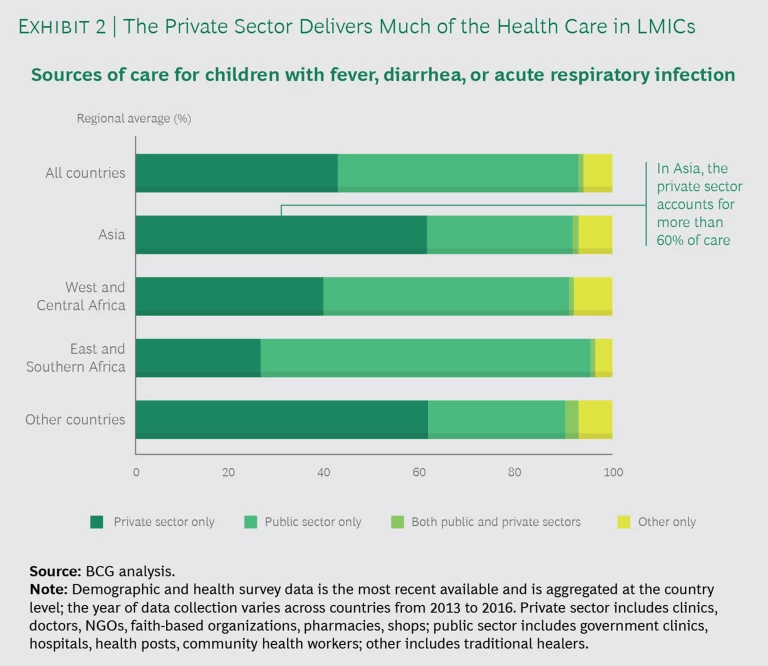
The private sector currently delivers 30% to 60% of health services across LMICs and often serves as the first point of care, but it tends to lag behind the public sector in quality and accountability. (See Exhibit 2.) The global health community has historically not focused on the private sector’s role in providing health care in LMICs. For example, WHO’s health delivery indicators track 42 metrics in the public sector but only 14 in the private sector. This is out of proportion to the private sector’s role in health care delivery around the globe. To drive progress against the health SDGs and improve health outcomes in LMICs, the global health community must engage in more strategic, thoughtful work with the private sector, including better leveraging of the private sector’s capacity and advantages while still ensuring quality and equality of access.
In South Africa, for example, the public sector is short-staffed in providing HIV services, with significantly fewer providers than recommended by WHO, while there are sufficient providers and capacity in the private sector to fill most of the gap. Improved collaboration between the private and public sectors could help many more patients receive quality HIV/AIDS treatment.
Similarly, in Indonesia, approximately 50% of tuberculosis patients receive care in private clinics or hospitals, yet historically the national government has had very limited visibility into the private-sector care pathway. The Indonesia National TB Program has begun to explore new ways to engage the private sector in finding missing cases, closing the gap in case detection, and improving TB care across the board. Through focus groups and other interviews, BCG helped identify several opportunities to make care in the private sector more efficient and effective, including adjusting incentives to ensure that patients receive care at the right level of the health system.
As these examples in South Africa and Indonesia illustrate, increased engagement with the private sector in LMICs can create important opportunities for greater scale, improved efficiency, and higher value for money in health care—all of which are critical to reaching the health SDGs.
4. Increase Global Health Financing and Maximize Existing Resources
Between 2000 and 2009, the annual growth rate of development assistance for health was 11.3%, but it slowed to just 1.2% between 2010 and 2015. With donor funds plateauing, it is critical for the global health community to both pursue new sources of financing and use existing funds far more effectively. Better use of existing funds can improve outcomes and make the case for more funding. A mix of approaches and financing mechanisms can be employed to ensure sufficient resources to support the health SDGs.
Experiment with results-based financing. Social impact and development bonds and other forms of results-based financing are increasingly used in high-income markets to finance education and justice reform initiatives, but they are still underutilized in low-income contexts, particularly in the health sector. Results-based financing has a mixed record in LMICs and continues to be debated, but there have been several successful examples in recent years. (See the sidebar, "How Elimination Bonds Are Being Used for Malaria.") For example, the Salud Mesoamérica Initiative used a national all-or-nothing performance award, which was then expanded in some countries to the facility level. As part of the larger initiative, this approach improved outcomes in prenatal care, contraceptive use, and skilled-attendant delivery in several countries in South and Central America.
How Elimination Bonds Are Being Used for Malaria
How Elimination Bonds Are Being Used for Malaria
Malaria elimination bonds are a good example of how results-based financing can be used in global health. Private investors or development finance institutions provide capital upfront to eliminate malaria in targeted LMICs. If the government or local stakeholders in the target country achieve previously agreed-upon performance metrics for malaria elimination, donors pay investors a return. If the country co-invests upfront, the pay-for-performance bonus incentivizes both country leaders and investors. This financing model is similar to development impact bonds but can also be structured to incentivize desired behaviors for eliminating specific diseases. The Inter-American Development Bank, the Bill & Melinda Gates Foundation, and the Carlos Slim Foundation have developed such elimination bonds as part of their Regional Malaria Elimination Initiative.
Leverage greater flows of private capital and blended capital. Private-sector resources and capital have been largely underappreciated and underutilized by the global health community to date. It is essential to increase incentives for private investors to invest in global health innovations, improve the visibility of global heath innovators in LMICs as potential investment opportunities, and develop more blended finance funds for health investment in LMICs. This approach is linked to results-based financing, since new financing instruments can attract new sources of return-seeking capital, including investors otherwise uninterested in global health funding.
With donor funds plateauing, it is critical for the global health community to both pursue new sources of financing and use existing funds far more effectively.
Increase domestic health spending in LMICs. To reach the health SDGs, many countries will need to increase their domestic health spending.
These are just some of the financing models and mechanisms that can enable progress toward the health SDGs. Not every model or source of funding described here will be suitable everywhere, but in all cases, countries will need to think beyond development assistance for health in order to meet the health SDGs.
5. Launch and Scale Innovative Interventions
Over the past several decades, the investment in infrastructure to deliver and scale vaccines, which are relatively system-independent, has brought significant benefits. By 2018, for example, eight years after the introduction of the meningococcal vaccine in sub-Saharan Africa, more than 300 million people affected by the disease had been vaccinated. In contrast, there have been few success stories in LMICs with the scaling of nonvaccine global health products and interventions, particularly those that are system-dependent.
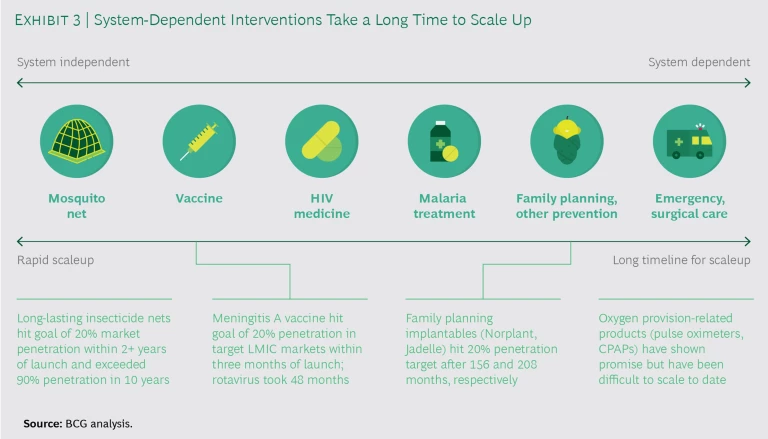
As noted earlier, by system-dependent interventions and products we mean those that are time-sensitive, logistically complex, and require highly skilled health workers. In contrast, system-independent interventions, such as mosquito nets, are less time sensitive, less logistically complex, and require less advanced skills. This distinction is important because system-dependent health interventions, like most aspects of maternal care, neonatal care, and surgical care, have proven far more difficult to scale—and scaling them will be critical in meeting the health-related SDGs. (See Exhibit 3.)
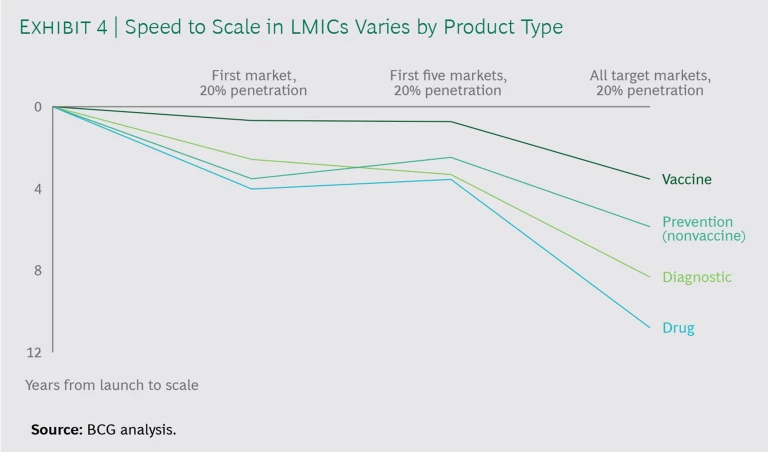
For example, it typically takes more than eight years for diagnostics and drugs to reach even 20% penetration across target LMIC markets. (See Exhibit 4.)
Research on the challenges of scaling system-dependent health interventions has yielded two key findings about what should be done differently in the decade ahead.
First, global health stakeholders must tap into the private sector's tremendous knowledge, capacity, and resources regarding the launching and scaling of products in new markets. While it is heartening to see more accelerators and incubators supporting innovators in low-income countries, few focus on the health sector. Even fewer effectively leverage best practices and tools from private-sector actors, particularly multinational biopharma and medical-device players, as well as consumer and tech companies, on how to reach scale in diverse LMICs.
Second and closely related, multinational health companies should be much more involved. To date, many multinationals provide their products in LMICs through partnerships with multilateral global health or other organizations. Often in these partnerships, the company produces and then hands over its product to its partner, which is then responsible for distributing it. But this approach fails to leverage a valuable asset of multinationals: their expertise and well-established processes for market entry, launch, and sales. In the years ahead, global health donors and foundations should focus much more squarely on launching and scaling products in low-resource contexts—and in doing so they should think about how to collaborate with and learn from large multinational health companies and other corporate stakeholders.
6. Pursue Next-Generation R&D
Next-generation R&D technologies primarily focus on products for high-income markets like the US, Europe, and Japan. But they could greatly benefit LMICs as well. For instance, in order to prioritize therapeutics with the highest probability of success, pharmaceutical companies are using predictive analytics to simulate a compound's interaction with the human body (an example is Schrödinger’s drug discovery platform, which uses predictive modeling and data analytics to rapidly develop therapeutics). This type of modeling could also be used with diseases like tuberculosis to accelerate a vaccine’s time to market.
Global health stakeholders must tap into the private sector’s tremendous knowledge, capacity, and resources regarding the launching and scaling of products in new markets.
Innovative clinical-trial designs, including adaptive trials, biomarker-led designs, and the use of surrogate endpoints, are increasingly helping to shorten drug development time—and regulators have signaled an openness to them. Whereas in 2010 the FDA approved 3 drugs in which a novel design had been used in clinical trials, in 2017 the agency approved 15 such drugs. The EXAMINE trial, for example, used an adaptive design, including an interim analysis, to compare an antihyperglycemic drug with the standard of care in reducing cardiovascular events in patients with type 2 diabetes. Inclusion of an interim analysis allowed investigators to evaluate and discontinue the trial, saving significant time and cost. Adaptive trials can likewise be used in low-income regions to save resources and time for drug development. Because LMICs are generally less profitable markets, more efficient trials are especially important, since they can de-risk and lower the costs of R&D, entice biopharma companies into the space, and stretch limited public and philanthropic dollars.
The SDGs are ambitious, to be sure, but we believe that significant progress can be made. We have the resources, capabilities, technology, and expertise to effectively pursue these goals—and we owe it to everyone around the globe to do better in achieving them. The opportunity areas highlighted in this report have tremendous potential to drive outsized impact and fundamentally change global health outcomes for the better in a cost-effective and efficient way.
The formula that worked for the MDG era will not hold for the SDGs. By investing in the right innovations and collaborations today, and by better leveraging the many tools and capabilities built over the past decade, we can dramatically improve health outcomes for many generations to come. By following this agenda, we have the opportunity to look back in the year 2031 at a story of success.