Even before the COVID-19 crisis hit, health insurers worldwide were struggling to keep pace with extremely rapid changes in the industry, including tighter integration into health care value chains, new technologies and geographic markets, and the shift to value-based care. The pandemic presents a far more immediate disruption, but one that will ultimately end. Moreover, it could actually present opportunities for insurers that have a strong market position and are willing to be bold.
We believe that success in the current environment requires that insurers understand the key trends reshaping the industry and then make strategic choices about how—and, equally important, where—to operate. Given the potential for reduced valuations, aggressive M&A could be a means to make faster progress in reshaping the portfolio and building key capabilities. Payers that can keep pace with rapid evolution in the industry will strike the rare balance of increasing revenue as well as customer satisfaction. Those that don’t will see the odds tip against them, possibly for good.
A Growing—and Increasingly Global—Market
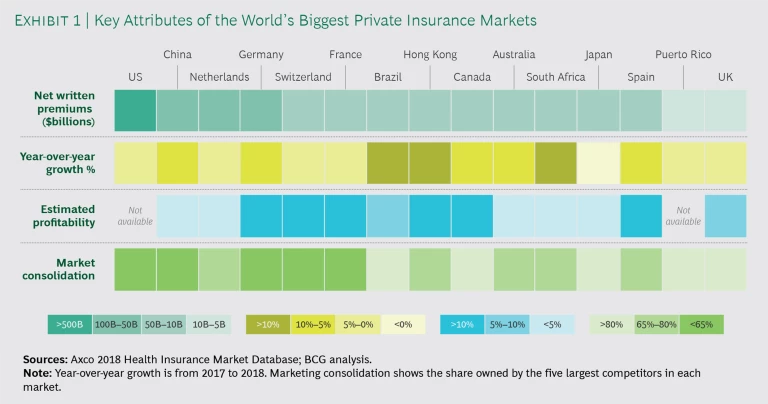
Over the past two decades, the global health insurance industry has grown significantly. The US continues to represent the largest share of the worldwide market (in terms of net premiums written), but some emerging markets grew at more than 20% a year between 2000 and 2017, including Singapore (22% CAGR), Saudi Arabia (23%), and China (26%). Strong trends spurring that growth include aging populations, a strengthening of health systems, and a growing middle class. In addition to strong growth and market sizes, as Exhibit 1 shows, many global markets show attractive profitability levels and low degrees of consolidation. Expanding into these markets allows insurers to access faster growth and diversify their portfolios in order to hedge risks more effectively.
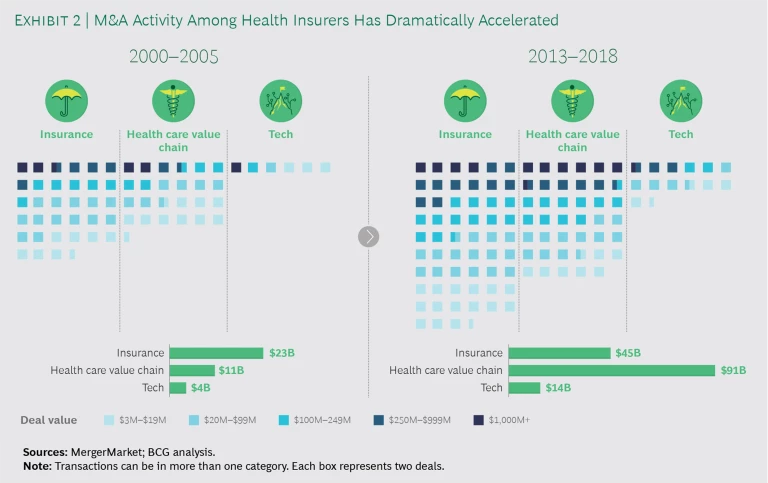
M&A has also been a key objective for health insurers. The past 20 years have seen an estimated $600 billion in deals related to the insurance sector. Many of those transactions were launched to consolidate and generate cost synergies. Since 2013, however, some of the largest deals were struck to help insurers expand up and down the health care value chain. The aim was to help insurers better deliver personalized, whole-person care, control rising health care spending, and give consumers more affordable plans and greater choice. A third category of deals has given insurers access to new technologies. (See Exhibit 2.)
Large-Scale Shifts in Five Key Areas
As significant as the changes in the industry have been over the past two decades, the future will see far more changes—and at an accelerating pace. We believe the following five shifts will create both challenges and opportunities for insurers.
Changing Demographics. First, the customer base for health insurance is growing. Populations are aging, particularly in developed countries. As a result, people will need more care—and often costlier care—for longer periods of time as they age. That will likely lead to increasing out-of-pocket or private health insurance spending in mature markets. In emerging markets, a growing middle class means that more people are able to access care and want to improve their basic health insurance coverage.
Digital, Data, and Analytics. A second major shift is the rise of technology in health care, especially new types of tools to gather and analyze patient data. Analytics are unlocking new models through which clinicians can deliver care, patients can be more directly involved in that care, and insurers can assess the value generated in order to determine fair reimbursement. And far more technology is coming. Consider that venture capital companies worldwide have invested about $17 billion across roughly 1,100 companies since 2010. These companies are developing new digital tools and solutions that will significantly alter value chains for both health care providers and insurers.
Consumerism. Health care value chains are changing, and patients today can play a direct role in managing their own care. Some of the largest potential opportunities lie in chronic conditions like diabetes. For example, patients can now be equipped with wearable devices such as blood monitors and insulin pumps that are linked to an app on their mobile phone. These devices allow patients to better monitor their condition, understand the implications of choices such as diet and exercise, engage more seamlessly with physicians, and—most important—avoid dangerous and costly complications.
The Shift to Value-Based Care. The challenge with the biggest potential implications for insurers is the transition from fee-for-service to value-based care. The health care industry still sees extreme differences in costs for a specific procedure, treatment, or drug—even in a single market—and outcomes are highly variable as well. Medical costs, already accounting for approximately 90% of premiums, continue to rise. Value-based care is a clear solution to these issues, but it represents a radically different approach for a health care industry that has multiple stakeholders and significant inertia, which hinders wide-scale change.
Disruption from New Market Entrants. Last, incumbent payers face a growing challenge from competition outside the industry’. For example, agile startup insurers are developing novel business models and customer propositions to take market share from established insurers. Similarly, tech companies are beginning to disrupt the health insurance market, seeing it as ripe for innovation. These players are benefiting from reduced barriers to entry, and they bring deep expertise in technology, consumer experience design, and retail, allowing them to develop more customer- friendly features and transparent processes.
How to Capitalize on Looming Changes
Any one of these shifts would pose a significant challenge to management teams. Collectively, they may seem insurmountable. However, winning insurers are not shying away from these trends but rather capitalizing on them by looking to enter promising new markets and building key capabilities. And they should use M&A to make faster progress in both areas.
Look to Enter Promising New Markets
Management teams need to increasingly focus on growth by expanding into new markets, factoring in the changes in demographics and market potential discussed above. We recently analyzed markets worldwide and broke them out into several dimensions. The fastest-growing countries for health insurers over the past several years include Vietnam, India, and the Philippines. We also identified markets with government policies that make them inviting markets to enter (Egypt, Kuwait, and Singapore) and those with the highest out-of-pocket spending, a promising indicator of untapped demand for health insurance (China, Japan, and Hong Kong).
That said, there is no single right answer for all payers. Rather, firms need to conduct their own assessment of markets, looking at several criteria.
Financial Attractiveness. Overall, payers need to use a range of metrics to assess the financial potential of a market. Baseline metrics include the aggregate value of net policies written, projected growth, and market profitability. However, payers should also look at other market factors, including out-of-pocket health spending per capita.
Current Capabilities. In addition, payers should filter markets based on how well they align with the organization’s current strengths, as those will likely produce the greatest revenue and cost synergies, potential for cross-market partnerships, and portfolio diversification.
Relative Difficulty to Enter and Operate. Finally, payers should look for markets that are not overly consolidated (defined as those where the top five players control less than 70% of total market share) and those where upcoming regulatory changes will create the most favorable entry opportunities. Another effective strategy for establishing a beachhead is to enter markets with an international private medical insurance offering specifically for expatriates.
Regarding how best to enter these markets, we expect that M&A will become increasingly relevant. In the short term, the COVID-19 pandemic is likely to dampen deal activity. But over the longer term, it could result in some assets coming onto the market at attractive valuations. Payers seeking to grow inorganically should ensure that they have capabilities in place to identify targets and conduct the requisite due diligence on them.
Build Key Capabilities
In addition to changing where they operate, firms need to improve how they operate—by building world-class capabilities in several areas.
Data Science. There is a large and growing body of cases that shows how payers are using data to make smarter and more objective decisions across functions. Data can be used to reduce costs across the value chain; one analysis found that by enabling smarter interventions, data science can reduce disease-related costs by 5% to 10%. However, data can also help payers better understand unmet needs of patients and providers and thus inform the development of new business models. Overall, insurers that have systematically adopted data science have improved profit margins by 2 to 4 percentage points, on a run rate basis, within two to three years.
Value-Based Health Care Models. Without intervention, health care costs will continue to rise, and patients will continue to experience wide variations in outcomes. To buck this trend, it is vital that insurers reform payments to create the right incentives for providers. One payer reduced overall care costs by 17% simply by reforming its payment approach in primary care, without any change in customer satisfaction levels. Quite simply, the most profitable insurers are those with the most creative and comprehensive approach to value-based care.
Digital Technology. New market entrants, as well as the top-performing global health insurers, are disrupting the industry with digital offerings. Basic measures online (or even mobile) claims, billing, and other administrative services; more forward-looking firms are able to digitize the entire customer journey, from finding a provider to booking an appointment, receiving results, and virtually every other aspect of the experience. Patients are seeing dramatically improved user interfaces in other industries and increasingly expect that in health insurance as well. (In fact, the best insurers treat them as customers, not patients.) Our research shows that payers can improve customer satisfaction ratings by 10% to 30% through digitization.
Capitalize on M&A to Make Faster Progress
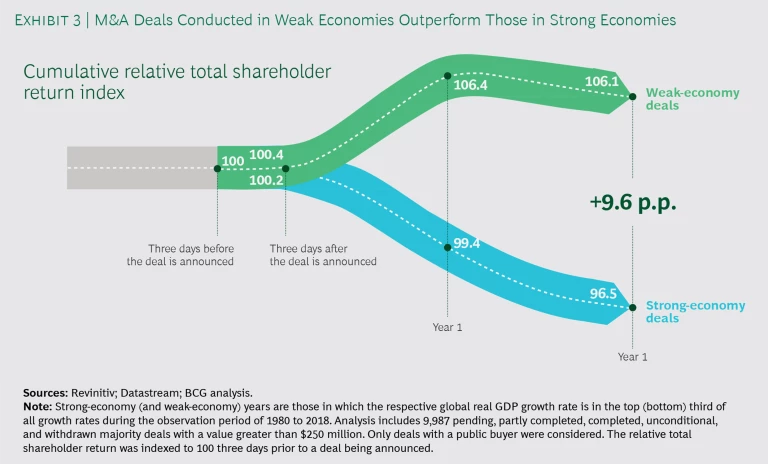
In both areas—expanding into new markets and building key capabilities—firms can make faster progress by using strategic M&A. The concept may seem counterintuitive during a period of COVID-related economic disruptions. But weak economies can actually be a good time for M&A. That’s particularly true for cash-rich companies that can take advantage of distressed valuations among targets operating in attractive markets and those with attractive assets and capabilities. BCG research has found that deals struck during weak economies can lead to better value creation—up to 9 percentage points in total shareholder return. (See Exhibit 3.)
The large-scale changes underway in the health industry—due to COVID-19 and other factors—are creating a future for payers that is part peril and part promise. In this environment, the top performers are relentlessly forward-looking. They take active steps to understand the challenges facing the industry in both the near term and long term, and they constantly seek to improve both how and where they operate, using M&A to gain an advantage. In a period of change and volatility, organizations that act boldly and seize the initiative will position themselves to thrive regardless of what the future holds.