As COVID-19 cases surge throughout much of the US and in many developing countries, the data on how to combat the coronavirus is becoming increasingly clear. In addition to wearing masks, limiting large indoor activities, and avoiding superspreader events, governments need to protect those whose health is most vulnerable by adopting a relatively affordable, high-ROI package of policy interventions. Protecting the vulnerable will give societies a path to contain the virus, reopen most businesses, and allow students to return to schools, without reverting to lockdowns. Pursuing this sensible path will produce better health, economic, and social outcomes at a lower cost than other options.
About 20% to 30% of the world’s population qualifies as health vulnerable, although the exact percentage varies by region and country. In the US, for example, about 20% of the population has chronic health conditions, and about 10% is generally healthy but over the age of 65. By protecting these people, governments can avoid severely straining their health care systems. For example, if the US adopted specific measures to protect residents of long-term care and other congregate living settings—people who account for less than 2% of the population and yet are among the most health vulnerable—it could prevent up to 9% of all COVID-19 hospitalizations. (See “The Quick Take.”)
The Quick Take
- We estimate that the five policies for protecting the health vulnerable could reduce COVID-19 hospitalizations by 40% to 65%. The monthly cost would be less than one-tenth of what the federal government in the US spent on its response during each of the first three months of the pandemic.
- The high end of our total cost estimate of $35 billion to $80 billion per month is unlikely to be reached, as governments can switch policies on or off in response to local levels of transmission, making the package increasingly affordable.
- Mask usage and increased testing are the two policies that will reduce hospitalizations the most; mandated mask usage is also the most cost-effective policy option. We estimate that if half of the health-vulnerable population consistently wore masks in public, it would reduce hospitalizations by more than 25%.
- To reopen schools and most businesses safely, governments must adopt the five policies for protecting the health vulnerable and maintain general policies for the rest of the public with regard to behavior, sentinel testing, limiting the size of indoor gatherings, and ensuring safe work practices. This combination of policies can contain the spread of infections and preserve ICU capacity.
On the other hand, if countries reopen without protecting the vulnerable, the health outcomes could be catastrophic. If schools and most businesses reopened in the US without taking steps to limit harm to vulnerable people, many places in the nation would run out of intensive care unit (ICU) beds in just weeks, and demand would peak at twice its maximum ICU capacity. This represents the national average; many localities would fare much worse during the peak period of hospitalizations.
It does not need to be that way. The most health vulnerable—people over age 65 with underlying conditions—are 30 times more likely to require hospitalization if infected than are previously healthy adults under the age of 65. They deserve government’s protection, and protecting them offers path to recovery that rejects the false tradeoff between lives and livelihoods.
Health-vulnerable people are not the only group that needs government protection. So do exposure-vulnerable people—those who are especially likely to come into contact with the virus. They disproportionately include minorities and immigrants who work in high-contact jobs and live in high-transmission neighborhoods .
Home, Work, Money, and Behavior
Home and work are the two primary avenues of infection for the health vulnerable, so policies must protect them in both places. Our models estimate that taking effective steps to protect the health vulnerable could reduce overall hospitalizations by 40% to 65% and cost governments far less than they have spent to date. For instance, the US—which authorized $3 trillion in government support during the first three months of the pandemic—could protect its health-vulnerable population for $35 billion to $80 billion a month. Moreover, it would probably not reach that $80 billion upper limit, as governments can spend less in areas that have lower infection levels. By cutting hospitalizations in half for this population, societies would have flexibility to manage the health consequences of the coronavirus and mitigate the risk of having to shut down a second time. (See “Our Methodology.”)
Our Methodology
Money alone is not enough, however. Governments also need to encourage changes in rhetoric and behavior. By designing smart programs and incentives, governments can enable and encourage the health vulnerable to physically isolate, to wear masks and other protective equipment, and to undergo frequent testing. Unfortunately, the opportunity to embrace these changes in behavior is quickly vanishing in the US and many developing countries. In some regions with high infection levels, it is already too late. Governments there must first enact swift, stringent lockdowns to crush the virus .
The Health Vulnerable
We segmented the health-vulnerable population into four groups on the basis of their risk of being infected either at work or at home. By “home,” we mean residence, which in some instances may be a long-term care facility, a dormitory, a prison, or some other congregate living setting.
Exhibit 1 identifies the four groups of health-vulnerable individuals:
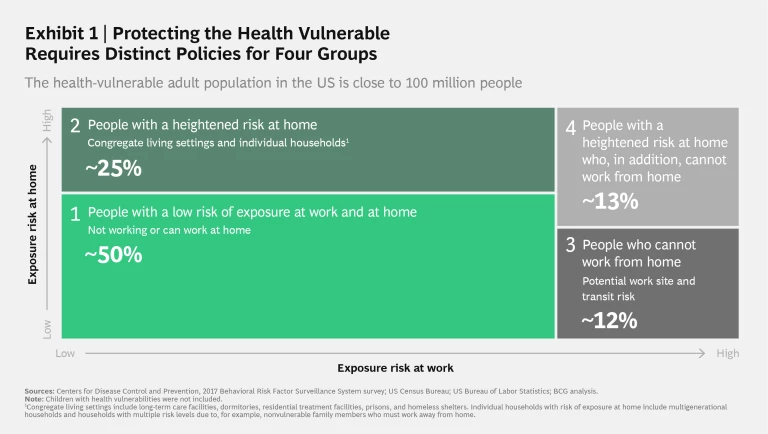
- People with a low risk of exposure at work and at home (a retired couple who live by themselves, for example, or a working-age adult with a heart condition who works from home)
- People with a heightened risk at home (for example, a nursing home resident, a migrant worker living in a dorm, or a diabetic adult living with a frontline worker)
- People who cannot work from home (for example, a hairdresser with respiratory issues, a medical staff member over the age of 65, or an immunocompromised factory worker with a long bus commute)
- People with a heightened risk at home who, in addition, cannot work from home (for example, a bus driver with a weakened immune system living in a multigenerational household in which other members work outside the home)
The good news is that the largest of the four segments—health-vulnerable people who do not leave their residences to work and who live in low-risk households—is the easiest to protect. Collectively, however, in the US, the remaining three segments are about as large as the first segment, and protecting them is a much bigger challenge.
Countries are starting to create policies to protect their health-vulnerable population in these settings. The UK, for example, provides food and mental health support to encourage sheltering in place among those who are safe at home and who do not work outside the home. South Korea has established a national monitoring system to keep residents at long-term care facilities healthy, and China requires health screenings in workplaces.
Many countries adopted these policies catch-as-catch-can—and despite the good intentions of those who crafted them, they have not necessarily worked at scale. Now is the last best chance to improve these policies, connect with hard-to-reach immigrant and minority populations, and encourage those at greatest risk of coronavirus exposure to shelter in place and stay safe.
A Policy Prescription
We have identified a package of five policies that collectively work toward protecting the four groups of the health vulnerable. (See Exhibit 2.)
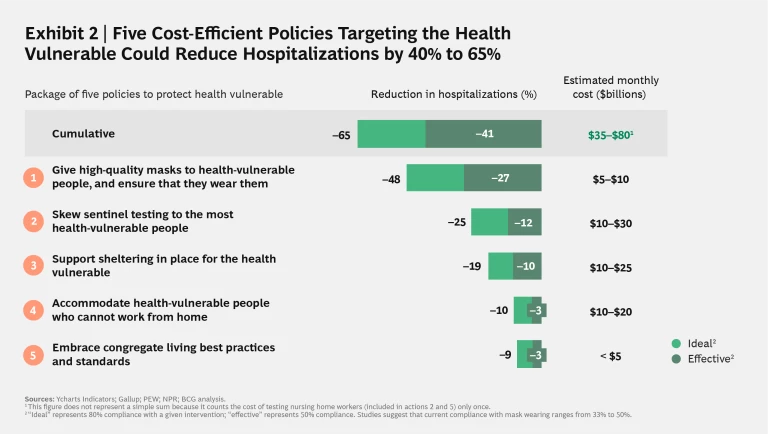
Masks and Behavior. At least in the US, wearing a mask has become a partisan political issue, but that distressing development obscures the fact that small changes in behavior can have an outsize effect in bringing the reinfection rate of the coronavirus below 1.0 so that the virus will eventually cease to spread. In one major metropolitan region that we modeled, a 9% shift by the public in compliance with social distancing and mask wearing made the difference between successful containment and an exponential outbreak. Governments should pay for masks for the health vulnerable and should design and execute behavioral campaigns to encourage the vulnerable to wear them.
Maskwearing is the highest-ROI policy. We estimate that if 80% of the health vulnerable wore high-quality masks in public, COVID-19 hospitalizations could fall by nearly 50%. Even simple face coverings are effective, especially in indoor spaces, where transmission is estimated to be 10 to 20 times higher than outdoors. They are also cheap. We estimate that this policy would cost less than $10 billion per month to reach more than 140 million health-vulnerable Americans and their family members.
Sentinel Testing. Testing has the second-highest ROI of the five policies and could reduce hospitalizations by up to 25%. In many regions, testing capacity is constrained, so establishing the right priorities is essential. The first priority is to test people with symptoms that are severe enough to warrant hospitalization and people who are in contact with confirmed cases. After dealing with those instances of urgent testing, governments should focus on sentinel or random testing of the health vulnerable and of those who are close to them—including workers, such as long-term care staff, who come into contact with them. Governments should also rapidly embrace pooled testing, a technique that combines multiple samples and tests them in a single batch, to stretch scarce resources.
Support for Sheltering in Place. This policy—which applies to all four health-vulnerable groups—aims to incentivize people to stay home by delivering resources to their door and combating feelings of isolation and loneliness while they stay home. Governments should encourage and incentivize companies to offer subsidized services—especially meal and grocery deliveries and online mental health consultations—to the health vulnerable. An 80% reduction from pre-pandemic levels in contact between the health vulnerable and the outside world could reduce hospitalizations by nearly 20%.
This policy is especially relevant for the elderly, who may need help in adapting to the online and contactless world. Because many people trust their faith communities, local nonprofit organizations, and peer groups more than they do their government, leaders should include these groups in planning and executing their shelter-in-place campaigns. The UK has adopted this approach and used it in delivering more than 1 million boxes of food. Ireland is investing in mental health services. In many countries, stores have set aside special hours for the elderly and the vulnerable to shop so that they can avoid large crowds. Depending on the level of local community transmission, this policy could be turned on and off as needed, making it even more affordable.
Accommodating the Health Vulnerable at Work. As lockdown orders have expired, workers have returned to jobs that require their physical presence, such as in stores, factories, meatpacking plants, agricultural fields, offices, restaurants, and amusement parks. Risks abound in these settings, as demonstrated by the outbreak in Europe’s largest meatpacking plant, in Gütersloh, Germany. In that instance, the failure of the private sector to protect workers and of the public sector to enforce worker safety boomeranged back to the general public, which was forced to live under a soft local lockdown after the outbreak.
The fact that 20% of the US workforce is health vulnerable poses a major challenge for public-sector and private-sector leaders. Governments and employers around the world have focused on such measures as testing and screening; safety protocols involving Plexiglas, protective equipment, and distancing; and staggered shifts. (See Exhibit 3.) Verizon, for example, has redesigned tasks such as broadband installation and in-store payments to minimize physical contact, and it has allowed call center employees to work from home during the pandemic. It has also extended sick leave policies and backup childcare.
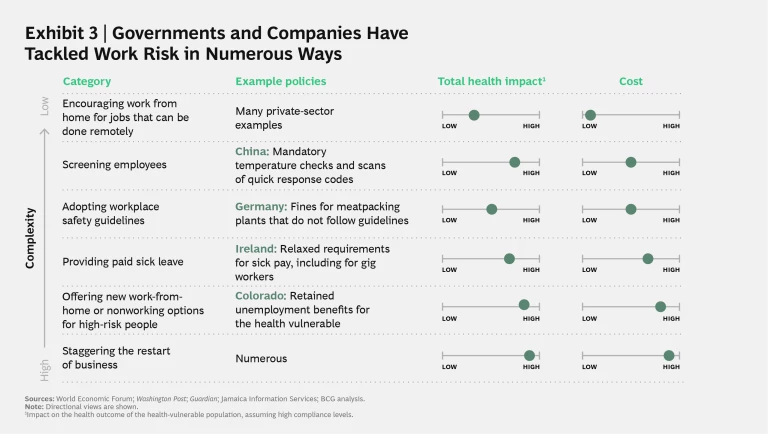
Government should encourage and incentivize the private sector, especially small and medium businesses, to follow the lead of Verizon and others. We know what works: adopting safety protocols and checks; enabling employees to move voluntarily from high- to low-contact jobs (from the cash register to the stockroom); and maximizing commute safety.
Colorado, a relatively healthy state, has approved extending unemployment insurance for the health vulnerable. Governments could direct unemployment insurance extensions to the highest-risk employees, a group that includes about 2% of the workforce in the US. Protecting these 3 million employees in this way would reduce hospitalizations as much as would similarly protecting approximately 80% of the US workers who are not health vulnerable.
Embracing Suitable Standards and Practices for Congregate Living. People who live in congregate settings account for a tragically large share of the death and suffering inflicted by COVID-19, despite amounting to a total population of less than 5 million in the US. Adding more protections for this group of people would cost less than $5 billion monthly and would reduce overall hospitalizations by up to 9%. The success of South Korea and other countries in dealing with this population provides real-world evidence of what works. In long-term care facilities, policies should rigorously limit outside visits, create spaces for quarantining, and test workers at least weekly. South Korea, for example, protects patients by closely monitoring the health and travel histories of staff and visitors and by incentivizing health and safety through government reimbursement. These policies have helped prevent new outbreaks.
Dormitories are an especially critical setting. Outbreaks have occurred in worker dorms, and colleges and universities that reopen in the fall will confront similar challenges in identifying, isolating, and treating infected students. Although relatively few college students are health vulnerable, they circulate in the broader economy and may have health-vulnerable family members.
The Policies Are Best Viewed as a Package
It may be tempting to treat these policies as a menu rather than a package, but they are complementary and mutually reinforcing. A health-vulnerable employee in a risky job, for example, would benefit from programs that encourage the vulnerable to stay at home as well as from programs that provide high-quality masks, testing, and social support. Testing alone—especially if it takes a week to receive the results—will not protect that employee. Stay-at-home pay would provide financial but not social and food support.
In the US, treating these policies as a package is especially critical now as the country confronts rising cases and pressure to reopen schools. Adopting them would provide the best path forward short of a full-scale lockdown. If governments can achieve 50% compliance, the package would allow the US to open schools and most businesses, although intensive-care units (ICUs) would still be at risk. (See Exhibit 4.) The US and other nations on the brink of health system overload must therefore take measures beyond just protecting the health vulnerable if they want to stay open while giving themselves a safer margin of error. Those other measures include general polices that should be adopted nationwide and specific policies aimed at the exposure vulnerable.
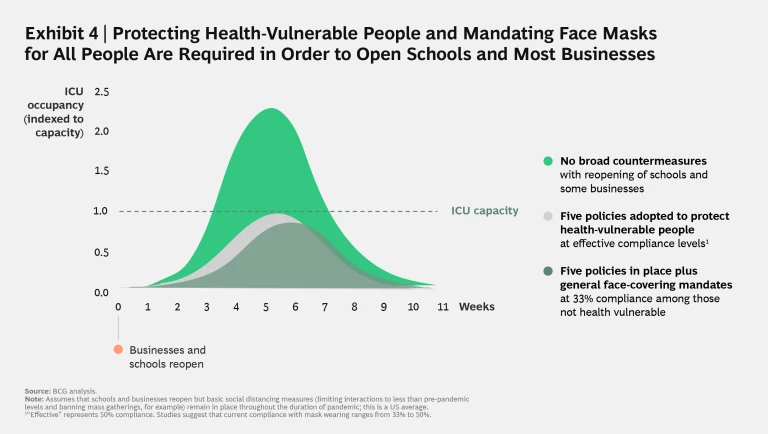
Combining specific policies to protect the health vulnerable and a general face-covering mandate would sharply reduce ICU demand if even one-third of people complied with the mask requirement. This would give hospitals the ICU headroom necessary to allow schools and most businesses to reopen without overtaxing the critical care system. Limiting large indoor gatherings and enforcing strong safety practices in the private sector are also vital to maintaining an ICU buffer.
To protect the exposure-vulnerable population, governments should prioritize sentinel testing in communities with large minority and immigrant populations along with smart outreach to those populations. Rhode Island, for example, does not require people to show a government ID in order to be tested, if they live in immigrant communities where the fear of authority is high. Many governments have begun to offer testing at community centers, houses of worship, and other places familiar to neighborhood residents. Ultimately, testing should be strategic, not reactive. Governments should also be using demographics and housing patterns to anticipate where future outbreaks may occur.
The virus has been wreaking havoc for more than six months, and it is not going away anytime soon. With cases surging in many regions, governments need an immediate, effective plan to return students to schools safely this fall and to reopen most business. We need to create a safer society and a stronger economy. And we need to get serious about racial and social justice. Protecting the vulnerable through this crisis accomplishes all three goals.
The authors would like to thank their BCG colleagues Kelsey Hayes, for segmenting the vulnerable and researching and costing the policies, and Lorenz Pammer, for modeling the progression of the disease and quantifying the impact of the policies.












