As health care systems and organizations plan for their recovery from the first wave of the COVID-19 crisis, they should not seek to return to their old ways of working. Instead, they should use the recovery as an opportunity to transform. This means building on the changes brought about by the crisis to enhance patient care and lock in operational improvements, while also managing the backlog of non-COVID patients and building resilience for future waves of the pandemic.
Time is of the essence in designing and implementing an effective recovery and reset plan. The next three to four weeks—while hospitals remain in crisis mode and countries progressively lift their lockdowns—provide a unique window of opportunity. Success requires an empowered frontline clinical staff that is working toward clear goals, as well as strong, executive-led governance.
Health Care Reimagined—in a Matter of Weeks
The pace and extent of disruptive change brought about by the crisis would not have been imaginable just three months ago. Since the pandemic erupted, health systems have implemented, almost overnight, many transformation initiatives (such as telehealth) that had been in the planning stages for months or years. They have also broken previously inviolable rules (regarding staffing ratios, for example), and they have radically redesigned ways of working (around subspecialty boundaries, for instance). These changes have led stakeholders to fundamentally reconsider both the speed and the degree of change that are possible.
Health systems have implemented, almost overnight, many transformation initiatives that had been in the planning stages for months or years.
Outpatient care is a case in point. After seeing relatively few advances in the past half-century, this area has undergone radical changes in just a few weeks—with providers adopting the type of front-end digital engagement that was already the norm in many businesses. Traditionally, hospitals have provided outpatient care through face-to-face appointments, and these services are notorious for their inefficient use of time and space. During the crisis, many hospitals and general practitioners have sharply increased the use of telehealth appointments. In the UK, for example, telehealth as a share of total appointments has increased from less than 1% to as much as 95% for some providers. In China, providers have set up an “internet hospital” to serve as an outpatient department. In other countries, hospitals have implemented centralized digital-triage processes that provide staff with symptom-checking tools, for example, and give general practitioners a hotline to access consultants, thus reducing the need for scheduled appointments. In a world with increasingly limited health care capacity, organizations will need to maintain these new ways of working in order to deliver care sustainably.
New approaches to cross-network coordination and communication likewise illustrate the breathtaking speed and scope of the transformation. To help balance patient load during the crisis, countries in Europe and Asia have set up rapid-transfer services to move patients between hospitals when capacity limits are hit. National health services have set up specialty hubs (such as the cancer care facility at the Royal Marsden Hospital in London) to treat non-COVID patients without exposing them to the virus. Secondary, tertiary, and community care services have increased collaboration in order to deliver care within the community whenever possible. These cross-organizational arrangements have sometimes resulted from stepping up collaborations that had been in development for years.
There are opportunities to accelerate additional changes at multiple levels:
- National and Regional: For example, taking a systematic approach to locating specialist services
- System: For example, driving the formation of integrated care systems and partnerships between hospitals
- Organization: For example, implementing new workforce models that encourage cross-training of staff
As they embed these improvements, however, health systems must mitigate the negative impacts of changes necessitated by the pandemic. Some measures have prevented patients from accessing the care that they need, putting their health at risk. In many systems, the new operating model is not sustainable. And across the sector, the consistency of standards and implementation may be falling short.
A Recovery and Reset on Three Dimensions
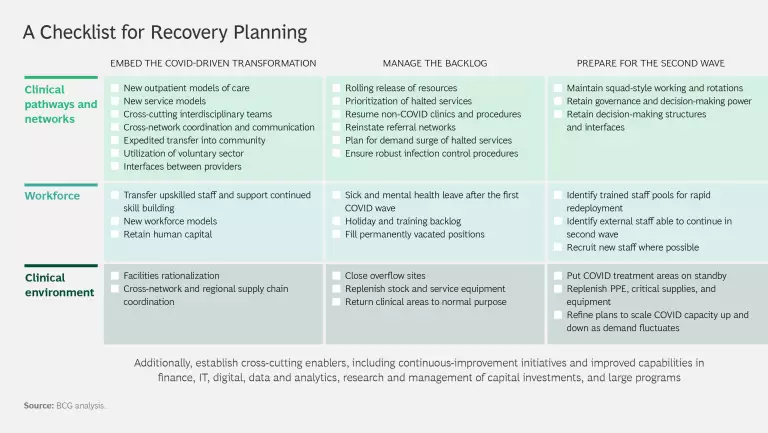
To ensure that the best changes are retained, health systems must take steps to lock in these improvements. Recovery planning should encompass three broad activities: embedding the positive aspects of the COVID-driven transformation, managing the backlog of non-COVID cases, and building organizational resilience for future waves of the pandemic. (See the exhibit for a checklist of specific actions.) All of these will involve clinical pathways and networks, the workforce, and the clinical environment.
Embed the COVID-driven transformation. As systems shift into the recovery phase, they must maintain the positive elements of the COVID-driven transformation while acknowledging that some of the new ways of working are unsustainable or pose too high a risk to quality. All hospital CEOs should work with their frontline staff to identify the changes that have and have not worked during the crisis. They should then plan five to ten high-impact initiatives and establish an agile program to embed those changes.
Manage the backlog. To free up capacity during the crisis, hospitals have delayed all but the most urgent elective procedures; some jurisdictions, such as New York, have canceled all of them. Around the world, hospitals have seen a significant drop in visits to emergency departments. In England, for example, these visits fell by 29% in March compared with the same month last year (including a 50% drop in patients with heart attacks). April saw an even bigger drop, with visits down by approximately 50% compared with April 2019. These figures suggest that patients are forgoing much-needed treatments, even at the risk of death.
Health systems need to address this backlog efficiently and systematically. That means prioritizing by clinical need, not just wait time, and planning for increased demand in specific areas (such as mental health). The demand for elective procedures will come at a time when infection control requirements are making diagnostics and surgeries more complex and difficult to perform, thus decreasing staff productivity. Improving efficiency while ensuring high-quality care will require a variety of new approaches, including load balancing and grouping together patients from multiple hospitals who require similar treatment, boosting productivity, developing new models of care, adopting a seven-day workweek, changing care protocols, and instituting new staffing models.
To ensure that the best changes are retained, health systems must take steps to lock in improvements.
Prepare for the second wave. Until a vaccine is available, there will be further waves of COVID-19 infections—it is only a matter of when and where they will occur and how severe they will be. Health systems around the world therefore need to build their resilience, incorporating the lessons learned from the first wave into new ways of working and business continuity planning. Critical-care capacity varies significantly among countries, and maintaining high levels of capacity is an essential element of preparation. In Europe, Germany has the greatest capacity per capita—seven times that of Portugal, whose capacity per capita is lowest. Along with its high rates of testing, Germany’s critical-care capacity may have been a contributing factor to its low COVID death rate. Health systems must also have in place the supporting structures needed—such as command and control, workforce models, the ability to transfer patients across networks, and strong links with community services—to ensure a flexible response to surges in demand.
How to Recover and Reset at the Right Pace
To pursue these imperatives, health care organizations must juggle several competing priorities: planning for recovery while continuing to treat COVID-19 patients; reinstituting previous transformation plans while pursuing new crisis-driven opportunities; and clearing the backlog while ensuring resilience for future waves.
To strike a balance among these priorities, organizations must answer a fundamental question: How do we want to use recovery planning to reach our target state? For organizations that had faced sustainability challenges or planned to undertake large-scale transformations before the pandemic struck, the best path forward may be to design a single plan that encompasses all aspects of the COVID-19 recovery. This will ensure a cohesive strategy for both recovery and transformation. Such a plan must incorporate three critical elements that proved successful in the COVID crisis: empowering frontline clinical staff, setting clear goals, and establishing robust but agile governance.
Health systems need to build their resilience, incorporating the lessons learned from the first COVID wave into new ways of working and business continuity planning.
Empower frontline clinical staff. Ensure that the frontline clinical community identifies and delivers the most valuable improvements, and break down organizational silos that impeded collaboration before the crisis. In order to maintain pace and engagement and ensure the success of recovery plans, clinicians need to be not only sources of ideas but also leaders of implementation initiatives. To guide them, provide clear and agreed-upon goals. And to ensure the right level of consistency, detail, and decision making with respect to the planned improvements, create multidisciplinary teams that include clinical leaders as well as leaders from operational departments, the program management office, and the executive team.
Set clear goals. Recovery and reset activities will range from short-term rapid–impact initiatives to more strategic and transformational long-term initiatives. Plan and implement these in parallel rather than sequentially. Select quick wins to pursue during the next two to four weeks; possibilities include telehealth for outpatient appointments, community collaborations, and critical–care capacity management. Take more time for longer-term initiatives, such as clinical facility configurations at a system level and specialty pathway optimization. These initiatives need to be prioritized and sequenced to ensure sufficient organizational capacity and delivery of the intended benefits.
Establish robust but agile governance. Most organizations have set up a command-and-control structure for their COVID response. This will likely need to remain in place for the short to medium term, not only to coordinate transformation and recovery activities but also to ensure that a governance structure is in place to manage future waves of the pandemic. Although this type of structure is well suited to day-to-day crisis management, it may not be able to manage all elements of a recovery and reset program. Recognizing this, many organizations have set up robust but agile executive-led governance for their transformation programs, closely coordinated with COVID governance. To ensure informed decision making and avoid a return to organizational siloes, the governance body should encourage multidisciplinary cooperation across clinical divisions as well as among operational managers and finance teams.
Recovery from the initial wave of COVID-19 presents a unique window of opportunity for the
health care sector
to truly and rapidly transform. There is a clear imperative to quickly develop group models across hospitals and to strengthen integrated-care systems. Those health systems that build the greatest resilience and agility will be the ones that not only recover from the acute crisis of the past weeks and plan for the short term, but that permanently change the way they work for the better.