Are we doing enough to protect the vulnerable? Several months into the COVID-19 pandemic, we are starting to understand the disease’s disproportionate impact on those who are over the age of 65, those with underlying health conditions, and socioeconomically disadvantaged groups.
With many countries and regions emerging from lockdowns and relaxing restrictions, it is timely and necessary to step back and ask about our national and regional COVID-19 strategies across the globe and prepare for future waves of infection. We believe that we must do more to protect the vulnerable, and in doing so, we will achieve better health and economic outcomes for the vulnerable and for society overall.
The three primary groups of vulnerable individuals are the following:
- Those Who Are Susceptible to Adverse Health Outcomes. People who are over the age of 65, individuals who have underlying health conditions, and those who are in both groups have a high risk of becoming infected if they are exposed to the coronavirus. In addition, if infected, these individuals have a high risk of experiencing adverse health outcomes. We call the people in this group health vulnerable.
- Those Who Are Vulnerable to Exposure. People, often racial or ethnic minorities and immigrants, have a high risk of exposure if, for example, they live in dense neighborhoods, crowded dwellings, or congregate facilities (such as long-term care facilities and prisons). People who ride mass transit or work in high-contact settings (such as retail stores and health care and long-term care facilities) also have a high risk of exposure.
- Those Who Suffer Economic Hardships. People whose livelihoods are affected by shutdowns or reduced demand (including those who work in such industries as food service, nonessential retail, and hospitality) have a high economic risk.
Recently, the discussion about how to best protect these vulnerable groups has become polarized. At one extreme, it is paramount to protect the first two groups using various lockdown approaches; at the other, restarting economic activity wins the day even if it increases infection and the risk of adverse health outcomes. We think this debate is fundamentally flawed on three levels.
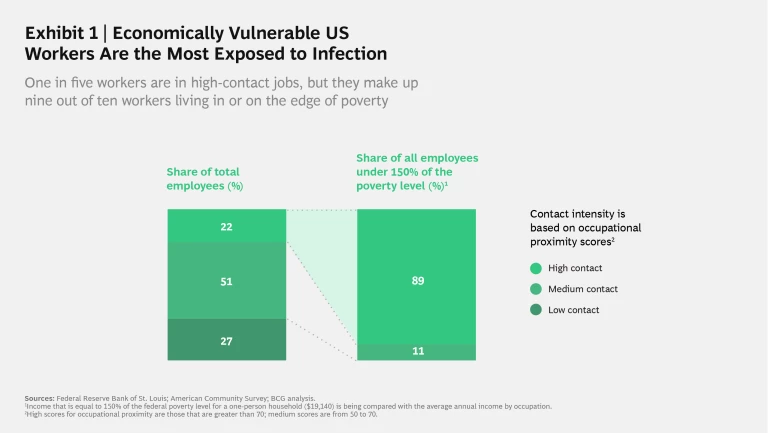
First, the vulnerable groups are not separate but overlapping. This has been true in Sweden, where Somalian immigrants make up less than 1% of the population but 5% of the cases; in Singapore, foreign workers, many living in crowded dorms, account for nearly nine of ten cases, although foreign residents make up only 20% of the population. In these cases, the workers are vulnerable to exposure, economic hardship, and potentially adverse health outcomes if they have underlying conditions. In the US, workers in high-contact industries, such as hairdressers and health care aides, make up 22% of the overall workforce but nearly 90% of low-income workers. (See Exhibit 1.)
These workers are more likely to have gotten sick or lost their jobs. And, if they live in multigenerational households, they are more likely to infect a parent or grandparent with heart problems. Given the overlap among those who are vulnerable to adverse health outcomes, exposure, and economic hardship, the coronavirus impact is disproportionately affecting already marginalized groups and exacerbating existing inequality around the globe.
In the US state of New Mexico, for example, indigenous Americans make up 8% of the population, but they account for more than half the COVID-19 deaths. Nationwide, Black Americans account for only about 14% of the US population but about 25% of COVID-19 deaths. This disparity echoes the racial justice inequities that have precipitated global protests in recent days.
Second, framing this debate as lives versus livelihoods reduces a complex, dynamic system problem to only first-order effects. For example, if a rapid reopening of the economy generates greater infections, overwhelms the health system, and causes numerous fatalities, consumer confidence will plummet, and parts of the economy will shut down with or without a government edict. On the flip side, the profound public health consequences of lockdowns also matter. The long-term mental and physical health consequences of unemployment, lost income, lost school days, and missed medical visits are real. The research into the number of deaths above normal levels is homing in on these consequences.
Third, the debate between lives and livelihoods is a false tradeoff. We need to protect those at risk of adverse health outcomes in order to protect the economically vulnerable. Why? Those over the age of 65 or with underlying conditions are 50 times more likely to require hospitalization if they are infected than healthy individuals under the age of 50. In other words, the infection of 1 million people who are over the age of 65 or who have underlying conditions would generate the same number of hospitalizations and roughly the same number of fatalities as 50 million healthy individuals. This fact has startling and largely unexplored implications for society and the economy. If governments significantly reduce the infection rate among the health vulnerable, they can widen their economic and health options to manage the coronavirus. We will explore a number of these implications over the coming weeks by examining the following:
- A deeper understanding of who is health vulnerable
- The ways social and economic support can be directed to those who are health vulnerable
- Improved measures for reopening the economy that better balance the needs of those who are vulnerable to adverse health outcomes, exposure, and economic hardships
Determining the optimal steps to manage the coronavirus are challenging in large part because the conclusive data is difficult to assemble. But we are learning more every day. The rest of this article examines how radically reducing the infection rate of those who are health vulnerable will allow economic and social activities to resume more swiftly and safely.
Why the Coronavirus Is Different
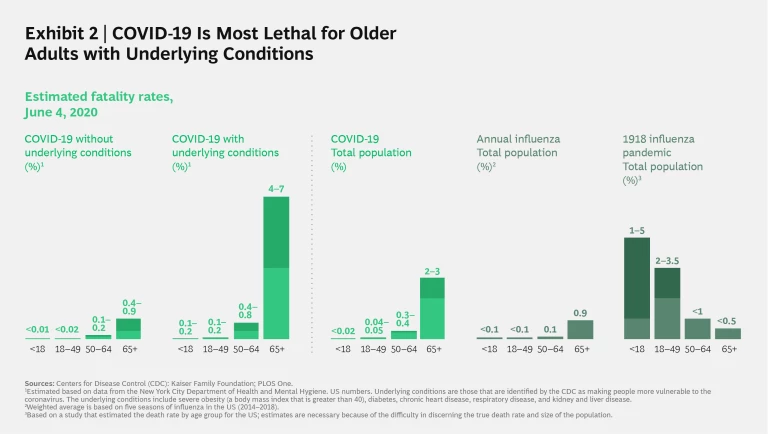
As a new disease, COVID-19 presents challenges. There is no preexisting immunity from past outbreaks. The long lag time between exposure and symptoms may allow individuals to unknowingly spread the disease. COVID-19 also has seemingly limited or no effect on most of its younger victims, despite its disproportionate effect on those who are over the age of 65, individuals who have underlying health conditions, and those who are in both groups. (See Exhibit 2.)
At the beginning of the crisis, when we knew far less than we do today, public health officials pursued a broad, cautious strategy that was based on past diseases in order to limit the spread of the coronavirus—notably, widespread lockdowns. The intent was to stop the coronavirus from overrunning the health care system and to buy time to prepare. That approach certainly made sense in places such as northern Italy and New York City.
Now that the coronavirus has been crushed in some places and contained or stabilized in others, we can employ an informed and focused approach that addresses the specific victims of the disease and that builds on what we have learned.
A Different Response
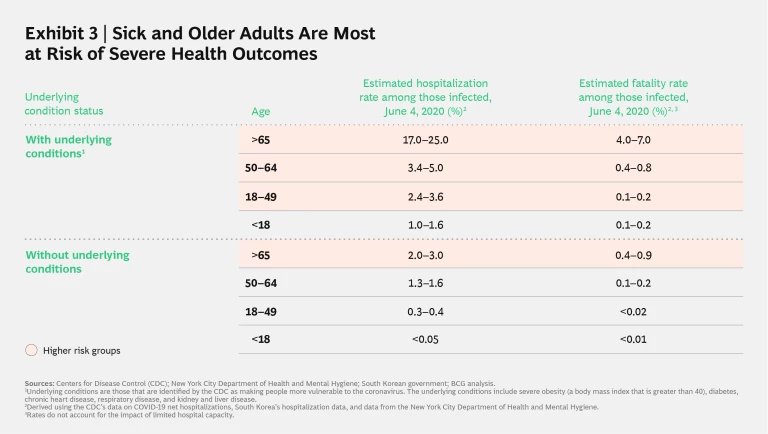
The world has refined its understanding of the disease in recent weeks. While there was a consensus early on that underlying conditions contributed to the severity of the disease and the risk of death, that contribution turns out to be even more significant than early estimates suggested. COVID-19 is especially lethal when it infects patients with underlying conditions, including severe obesity, diabetes, chronic heart disease, respiratory disease, and kidney and liver disease. (See Exhibit 3.) At one extreme, 17%–25% of infected people over the age of 65 with underlying conditions enter the hospital. At the other, less than 0.4% of those who are healthy and under the age of 50 land there.
Many governments have tried to protect those who are health vulnerable. Israel engaged guards to enforce its strict lockdowns at long-term care facilities and provided isolated beds for sick residents in geriatric rehabilitation centers. France is offering free transportation and priority shopping lines to workers with high exposure risks, and it has created specialized medical sites for homeless populations to quarantine and receive care. Singapore moved 2,000 nursing home employees into separate hotels to prevent the spread of the coronavirus.
The data shows that these efforts are not sufficiently widespread. If we had been effectively protecting those who are health vulnerable, we would see lower infection rates among this population. Tragically, that is more the exception than the rule. A study of eight countries’ long-term care facilities showed that these facilities accounted for anywhere from 19% (Hungary) to 62% (Canada) of COVID-19 deaths. In New Jersey, the second hardest hit state in the US, more than half of deaths occurred in long-term care facilities. Some estimates suggest that these facilities are home to more than 40% of US COVID-19-related fatalities, despite their residents accounting for about 0.5% of the overall population. This would suggest that residents at these facilities are being infected at a rate that is at least three times that of the general population—and perhaps much more.
Those over the age of 65 and with underlying conditions outside of long-term care facilities are also at great risk. For example, more than 95% of hospitalizations in Austria have been individuals over the age of 65 or people with underlying conditions. In South Korea, individuals over the age of 60 have accounted for more than 90% of COVID-19 deaths but less than 25% of confirmed cases.
In an ideal world, we would seek to minimize hospitalizations of all individuals, not just those who are health vulnerable. But at this moment, protecting the health vulnerable is emerging as the best way to improve overall health outcomes, reduce hospital burdens, and increase economic options.
A Shift in Strategy
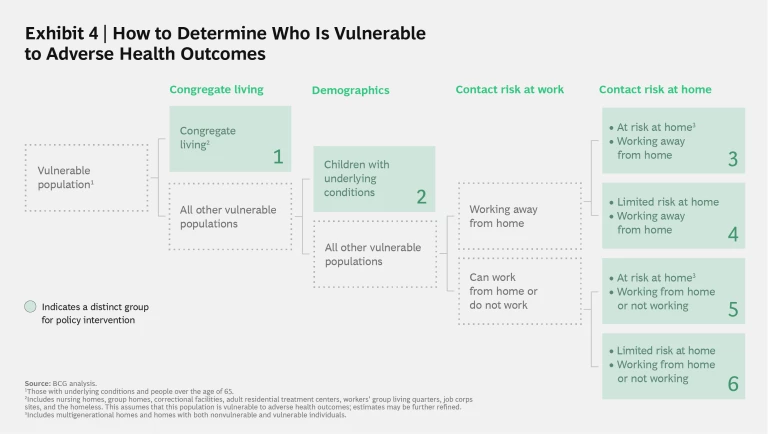
Effective strategies to protect the health vulnerable will require that societies help them limit their exposure at work, home, school, and especially congregate living situations. (See Exhibit 4.) For the highest-risk populations, support for extended sheltering in place also may be necessary. Across the world, we have already lost hundreds of thousands of individuals who were the most health vulnerable. The tragedy at long-term care facilities suggests that we remain a long way from protecting our most health vulnerable.
We must take collective actions to drive better health outcomes, protect our hospitals, and potentially give us better paths to enable our children to return to school, let local businesses reopen safely, and resume daily life. Here are some questions we should consider:
- How can scarce testing and tracing capacity be shifted in order to identify community spread in health vulnerable populations?
- What additional support can be extended to health vulnerable individuals who are unable to work from home?
- Are there innovative wraparound services, including mental health counseling, that can be provided to individuals who are sheltering in place for an extended period?
- How can we enable separate housing solutions for high-risk individuals that live in households where other family members are at high risk for infection?
- Opening the lens to the broader population, how can we curtail superspreader events and create national campaigns to maintain and improve existing prevention protocols, such as hand washing and mask wearing?
We will explore specific policy ideas for these in subsequent posts, including how the protection of those who are health vulnerable fits within a broader framework of protecting those vulnerable to exposure and to economic hardship.
If we collectively protect the vulnerable, we will protect all of us.
Let’s discuss. Please share your thoughts with us at covidresponse@bcg.com .
Disclaimer
Disclaimer
The situation surrounding COVID-19 is dynamic and rapidly evolving, on a daily basis. Although we have taken great care in the preparation of this article, it represents BCG’s view at a particular point in time. This article is not intended to: (i) constitute medical or safety advice, nor be a substitute for the same; nor (ii) be seen as a formal endorsement or recommendation of a particular response. As such you are advised to make your own assessment as to the appropriate course of action to take, using this article as guidance. Please carefully consider local laws and guidance in your area, particularly the most recent advice issued by your local (and national) health authorities, before making any decision.