By narrowly focusing on Black hesitancy in the early rollout of COVID-19 vaccines, the US missed an opportunity to create an equitable distribution plan. It’s not too late to flip the script and save lives of a community disproportionately devastated by the pandemic.
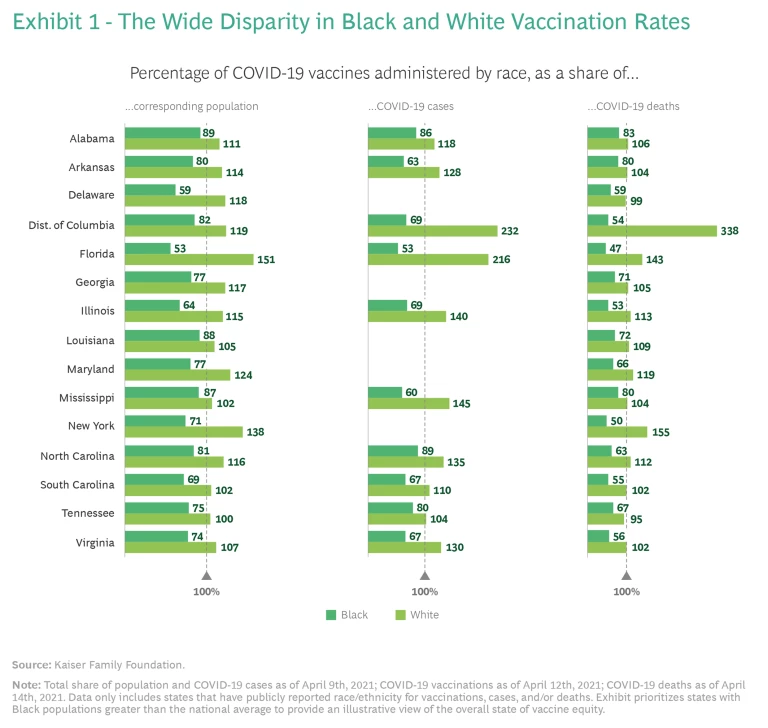
Racial inequity has been an enduring feature of the COVID-19 pandemic from the beginning—and it continues as the US tries to contain the virus through vaccination, with white people being vaccinated at far higher rates than Black people.
Myths about the causes of these racial inequities have persisted as well. In the early days of the pandemic, a common misperception was that Black people in the US were much more at risk for adverse outcomes due to poor underlying health. That was proven not to be a primary factor . Black people suffered worse outcomes because they were more likely to be exposed to the virus—from employment in essential jobs, from living in multigenerational households or hard-hit nursing facilities, or from having even less access to testing than white people.
More recently, the belief that Black people are more hesitant than white people to be vaccinated became a central part of the public narrative. This sentiment had validity six months ago, when the vaccines were still under development. A Kaiser Family Foundation (KFF) poll last October showed 49% vaccine hesitancy among Black people in the US, far higher than the hesitancy of white people. However, more recent surveys by KFF, Marist University, and BCG show little difference in hesitancy between the two groups. BCG’s most recent US Vaccine Sentiment Survey , completed March 16–21, showed that 18% of Black people said that they would not be or were unlikely to be vaccinated, only 2% higher than the share of unwilling or unlikely white people.
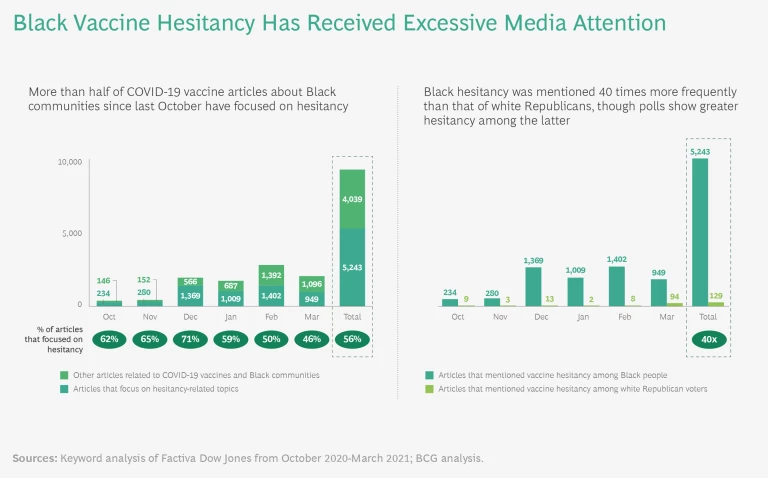
Nevertheless, as early as December—when polls already were reporting little difference between Black and white hesitancy and the vaccine rollout had started—media coverage of Black hesitancy began to spike. (See “The Media Misses the Mark.”)
The Media Misses the Mark
During that same period, other vaccine-hesitant groups were receiving far less attention. Black hesitancy was mentioned 40 times more often in written news coverage than, for example, white Republican voter hesitancy—even though multiple polls by reputable pollsters dating back to August have shown greater hesitancy among white Republican voters than Black people. As recently as March, articles mentioning Black hesitancy dominated white Republican voters’ hesitancy by a factor of ten.
The consequences have been significant. The hyper-focus on Black hesitancy was reflected in decision making with respect to resource allocation and vaccine rollout. Resources—especially early on—were largely deployed toward providing information and education to combat hesitancy rather than being directed to ensuring that the vast majority of Black people who were willing to be vaccinated would be vaccinated. Resource allocation and related activities did not sufficiently evolve over time to reflect the data showing a rise in vaccine confidence among Black people. These decisions have surely contributed to the wide disparity in vaccination rates for Black and white populations in the US. (See Exhibit 1.)
Longstanding healthcare inequities have also played a role. Because the US was in a public health crisis, and needed to act swiftly to save as many lives as possible, it chose to funnel vaccines into preexisting, high-throughput systems that catered to those who historically have been well served by the healthcare establishment. For example, systems favored those with online access to search for vaccination availability, flexible employment that enables midday appointments, and transportation to sometimes distant vaccination sites. These established systems favored white people more than Black people—exacerbating a pattern of inequity seen in the declining share of resources devoted to public health and other measures.
In addition, the early vaccination criteria based on age and preexisting conditions further favored white people, despite higher rates of exposure and mortality in Black communities. Adjusted for age, for example, Black people are two times more likely to die from COVID-19 than white people.
Vaccines have been funneled through preexisting health systems, exacerbating long-established patterns of racial inequity.
While these decisions may not have been intentionally exclusionary, they had that effect by catering to those perceived to be easiest to reach without specific consideration for those with higher infection and death rates. It would have been possible to go full speed and reach the millions of Black people eager to roll up their sleeves; the fact that we’ve succeeded at the former while largely failing at the latter reflects inertial planning and decision making, which are rooted in a larger failure to understand the racial inequity built into our nation’s health system.
Achieving speedy, high-throughput vaccine administration while ensuring equitable vaccination rates requires an intentional focus to overcome long-established practices, policies, and infrastructure. Nearly five months into a nationwide vaccination campaign, it is not too late for the US to flip the script.
Getting Equitable Access Right
While addressing the remaining portion of the hesitant population is important, the overwhelming focus on Black hesitancy continues to distract from where attention is most needed: access. Federal, state, and local governments must commit to ensuring equitable distribution and administration by resolving the perceived tension between simplified, centralized approaches and more diversified, place- and population-based efforts. While it is important to run well-functioning megasites that vaccinate thousands of people a day, as some cities and states have done, that is insufficient. We need to bring arms to vaccines and vaccines to arms by placing sites in historically underserved communities, and by running operations focused on reaching Black and other target populations.
High-volume megasites are important, but they aren’t enough.
The last mile is incredibly difficult to organize for public health officials, who are under-resourced and accustomed to operating in a top-down, emergency-response mode. These officials will need to engage with new partners, fund flexible microgrant programs, and create communication channels. Community and stakeholder engagement amid a pandemic is challenging but necessary.
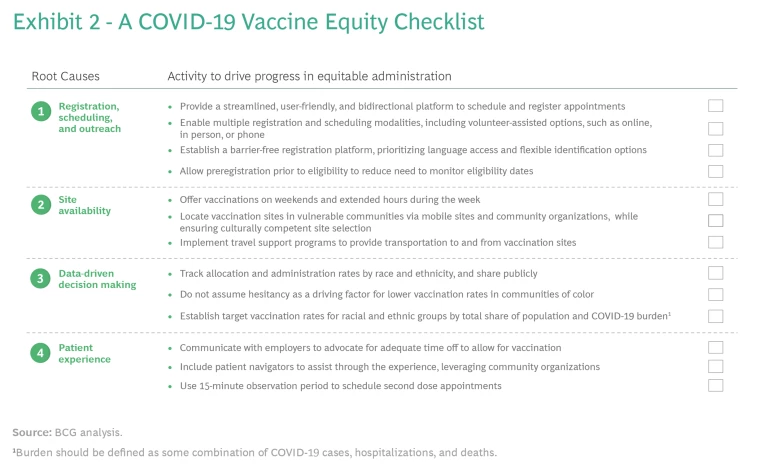
We suggest a last-mile approach consisting of small, local sites and larger mass-vaccination sites with extended hours, reserved windows of time for select zip codes or neighborhoods, and the availability of ride-sharing vouchers. Governments at the federal, state, county, and city level have begun this work, but there is far more to do. In our conversations with more than 150 community leaders nationwide who actively work in vaccine distribution, access, and administration, we uncovered four key root causes for inequitable vaccine access:
- Registration, scheduling, and outreach. Individuals are unable to register for or schedule vaccination appointments online. Vaccination sites are not conducting community outreach to schedule appointments.
- Site availability. Site locations often have poor public transit options and are located far from predominantly Black neighborhoods.
- Patient experience. Many Black people do not have flexible employment and childcare options. Unpredictable wait times add to the uncertainty and exacerbate the challenge. Even if they overcome these logistical challenges, many Black people have a justifiable mistrust of health care systems and may be unfamiliar with navigating them. Most vaccination sites do not address these concerns through culturally competent engagement, care, and easy navigation.
- Data-driven decision making. Few vaccine sites have captured and reported rigorous data on vaccination by race. Most of the research is based on sampling or statistical modeling rather than comprehensive data visibility and transparency. If we don’t capture real-time data related to equity, we can’t improve it.
In an effort to address these four root causes, we drafted a checklist that can help the administrators of vaccines (local jurisdictions, community- and faith-based organizations, and health providers, for example) ensure that they are doing everything possible to achieve equitable vaccine access and administration for Black communities. (See Exhibit 2.)
The checklist is simple; execution of it is not, because it requires officials to tackle all four root causes at once. Piecemeal approaches are doomed approaches. Supplemental materials with practical advice on how to build systems that are both fair and fast, along with brief case studies of organizations that are successfully addressing the root causes of inequitable access, can be found here .
About one third of the US population is fully vaccinated, which means we still have the potential to correct the inequities of the first four-plus months of rollout. Our colleagues estimate that 65% of the population will need to be vaccinated to reduce the disease burden of COVID-19 to the level of the flu. If that 65% is disproportionately white, the pandemic will not yet be over for members of minority communities, who will continue to be at greater risk of infection and saddled with limited economic opportunity.
We are no longer a supply-constrained country. Our US Vaccine Sentiment Survey suggests that without improving access and acceptance, only 55% of the US population will be vaccinated. Our focus needs to be on generating demand. As we work our way up the demand curve, however, the temptation may yet again be to turn our attention away from access on the theory that generating demand requires more public service announcements, advertising campaigns, and other messaging.
As we work our way up the demand curve, we must continue to invest in access.
While these approaches have a place, they aren’t enough. Investing in access to vaccines will also improve demand and uptake among those who want the vaccine but have not been able to get it yet. Studies have repeatedly shown that knowing somebody who has been vaccinated encourages the hesitant to roll up their sleeves.
Community leaders have recognized the importance of providing equitable access and implemented models to do just that. Examples include:
- The Choose Healthy Life Black Clergy Action Plan, which established a national council of faith-based leaders, chaired by Rev. Al Sharpton and Rev. Dr. Calvin O. Butts III, to conduct vaccine outreach and COVID-19 testing in 50 Black churches across five pilot cities, and held successful vaccination events in New York City and Newark.
- Civic leader Cora Masters Barry, who, in collaboration with the Rodham Institute and other Washington, DC, leaders, held an exclusive vaccination pop-up event called “Don’t Miss Your Shot” for residents of Ward 8, administering over 850 vaccines in a single day.
A Platform for Health Equity
The US will eventually win the fight against COVID-19. All pandemics eventually end; how it ends matters, though. We must acknowledge the systemic racial inequity in our health care system and take this opportunity to combat it on behalf of Black people and all communities of color. Perpetuating myths about Black vaccine hesitancy only makes this work more difficult. By blaming the victim rather than a health care system that has insufficiently served minority communities during the pandemic, officials are failing to protect the people whose lives and livelihoods have been most disrupted by the virus.
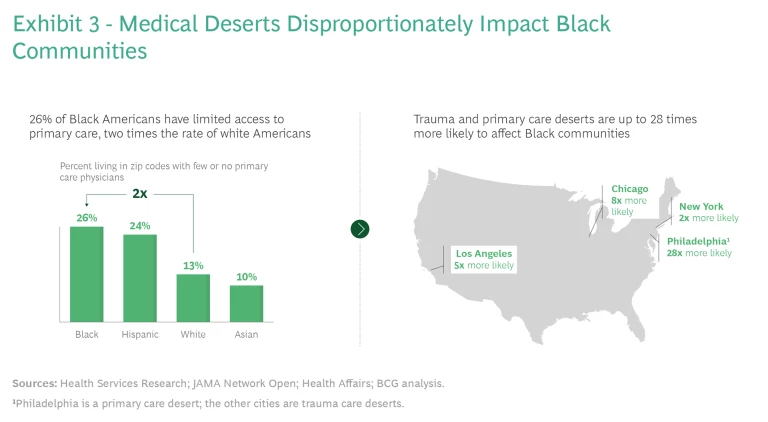
It’s not too late to build equity into vaccination rollout campaigns, but if we stop there, we will have lost an opportunity to make progress on the broader issue. We can use the design of these campaigns to create more equitable health care systems. It may be tempting to view the defunding of public health over the past two decades, the existence of “medical deserts” with limited primary care options in minority communities, and the tragedy of COVID-19 in those same communities as isolated events. (See Exhibit 3.) But they are part of the same problem.
If the pandemic ends without the US laying the foundation for a better and more equitable health care system—or at least the understanding of how to build it—we will have failed the people most affected by it.