To deliver superior outcomes at scale, companies need to invest in ecosystems. Forging strong connections with patients and partners will be key.
Thanks to emerging digital technologies, companies across the health care industry —including software and service providers—now have the means to dramatically improve patient outcomes. But, so far, there has been success only in pockets. Most companies have struggled to scale or make direct patient impact, often because they innovate in silos without sufficiently connecting with the patients they are innovating for or with the partners that can provide missing capabilities.
To leverage the digital opportunity fully and create transformative change, health care innovators must address needs across the patient journey. A winning formula is to create a robust health tech ecosystem, for which three types of connections are key: with patients and practitioners, with ecosystem partners, and within the organization itself. Pear Therapeutics, Omada, Click Therapeutics, and other health tech companies that have recently taken this path have already made important strides forward.
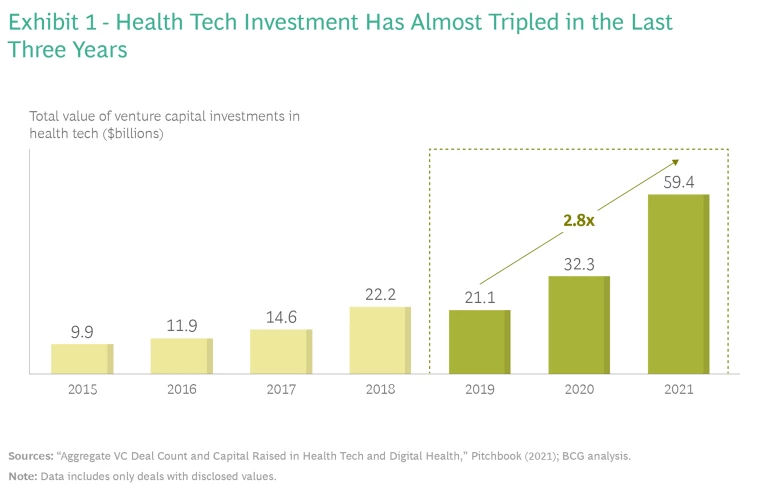
Health Tech on the Rise
The past few years have brought significant growth in health tech across digital health solutions, platforms, software, hardware, data, and artificial intelligence to solve medical problems and improve patients’ lives. This surge of advancement is only just ramping up, as evidenced by recent growth in venture capital investment. (See Exhibit 1.)
BCG’s recent survey of
health care providers
suggests that digital adoption will continue well beyond the resolution of the pandemic. Four out of the top five engagement channels are virtual, with rising effectiveness since May 2020, and more than 70% of physicians said they plan to keep or increase their telehealth usage as the pandemic subsides.
Remote health
is here to stay.
Connecting with Patients and Practitioners
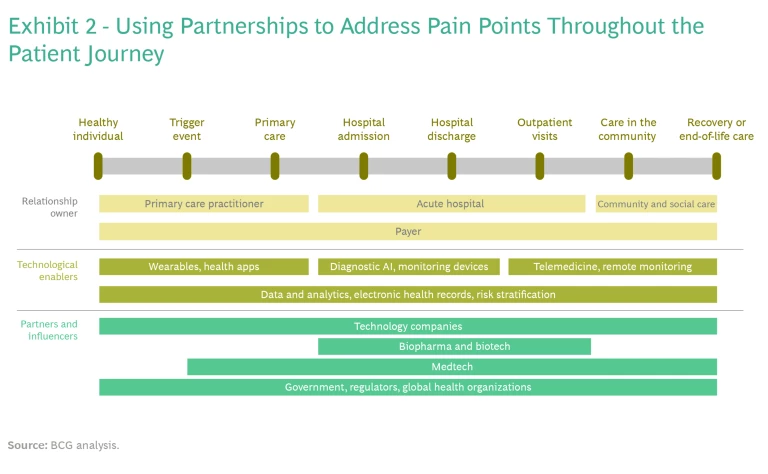
The development of any impactful health care innovation begins with the patient. Consequently, any company that wishes to create real change first needs to look at the entire patient journey and identify the various pain points that occur along a treatment pathway. Companies can use this information to determine what solutions need to be built or altered to deliver the most impact for general, acute, and chronic conditions.
Digital therapeutics and telehealth companies can, for example, contribute to solutions more effectively than ever before by leveraging data now available from wearables and other digital sources. These technologies can drive deeper insight, influencing patient behaviors to prevent and manage chronic conditions. Livongo, a digital therapeutics player focused on diabetes care, has combined blood-glucose-measuring technology with a data-driven app that patients can use to manage their diabetes in real time.
Patient input is also a valuable source of insight that providers are utilizing to personalize solutions and gain critical feedback on the impact treatments can have on quality of life. Gilead Sciences has launched the PrEP hub, a digital platform that tailors HIV care pathways and education materials in response to patient feedback. On Epsy, a digital epilepsy platform, patients can log information on seizures, medications, and more to get a better understanding of their conditions. The platform also allows patients to share their data with physicians to understand the impact of therapeutic treatments and optimize their efficacy.
When addressing pain points along the patient journey, companies must also consider the needs of practitioners because of their direct impact on patient health. Practitioners increasingly rely on data and analytics to make sound diagnoses and on telehealth to improve patient access and reduce operating costs. They also rely on remote-management technologies (such as symptom trackers, monitoring devices, and patient dashboards) to keep an eye on patients outside of the traditional care setting and to avoid costly treatments, from emergency procedures to hospital admissions. For example, three South East London hospitals are using remote-monitoring technology provided by the NHS to monitor patients with rheumatoid arthritis at home and to reduce hospital visits.
Like patients, practitioners play an important role in the development of new solutions. Their perspectives are critical for ensuring that a solution meets clinical safety standards while impacting patient outcomes. Omada Health, for instance, actively involves clinicians in the development of its minimum viable products (MVPs)—so much so that the company has renamed it the minimum clinically viable product, or MCVP.
Connecting with Partners
Companies that focus on solving specific needs for patients or practitioners can certainly be successful. But to transform health care at scale and carve out sustainable advantage, organizations need to address a broader set of pain points, effectively creating a seamless patient journey.
Since no company has the offerings, capabilities, or access to patients or providers to cover the entire journey at scale, it’s critical to partner with players who own parts of the journey that others cannot easily address themselves. (See Exhibit 2.)
Winners in this space have spent the past few years building ecosystems with the patient journey in mind. For example, Pear Therapeutics, which develops prescription digital therapeutics for serious illnesses, has forged partnerships with Intellectual Ventures, USC, SickKids (the Hospital for Sick Children), Apricity Health, and clinicians across the US.
The shift in focus to a digitally enabled patient journey requires organizations to rethink the internal connections required for innovation.
Organizations are also partnering with Big Tech to leverage their advanced data collections, digital capabilities, and infrastructure. Moorfields Eye Hospital’s Biomedical Research Centre has partnered with Google’s AI unit, DeepMind, to create a tool that helps prevent the progression of serious eye disease. Using Moorfields patients’ eye scans, DeepMind is developing an algorithm that can predict whether people with age-related macular degeneration in one eye will develop the condition in both eyes, so that they can be treated beforehand.
Connecting Internally
The shift in focus to a digitally enabled patient journey requires organizations to rethink the internal connections required for innovation. The traditional set of participants and ways of working won’t suffice when innovation cycles last weeks instead of months or years.
Developing good products for patients requires robust, cross-functional, and agile ways of working , with frequent iterations and user testing. It also requires a much more diverse set of skills, such as user-centric design, risk-based legal and compliance approaches, data science, and machine learning.
In the near future, the nature of competition in the health care industry will change. Instead of companies vying with peers, whole ecosystems will compete to deliver an optimized patient journey and better outcomes at scale.
To build solutions in fast update cycles—a key to competitive advantage—agile development teams need to work in the field with patients and clinicians to understand the causes of key therapeutic delivery frictions. This approach is very different from more traditional, expert-led approaches to R&D. By combining these two ways of working, organizations can bring the best of R&D expertise and user-led design thinking together to create an optimal solution.
Take, for example, Geisinger Health, a US-based integrated health system with approximately 55 clinical sites. Working with patients, functions from across the organization, and ecosystem partners, Geisinger uses agile, human-centered approaches to develop and implement new digital products and solutions such as EDGE, an innovative asthma management system.
Building a Winning Ecosystem
In the near future, the nature of competition in the health care industry will change. Instead of companies vying with peers, whole ecosystems will compete to deliver an optimized patient journey and better outcomes at scale. Organizations that come together to build winning ecosystems will have keys to the digital front door: ownership of the patient relationship.
To create a winning ecosystem, it’s important to pick winning partners. In addition to doing the usual due diligence , organizations need to select players that have developed leading solutions for a pain point that needs covered or those with unique technical expertise.
Intermountain, a nonprofit integrated care system, has built a winning ecosystem in this vein. Intermountain’s partners provide clinics, a medical group, affiliate networks, hospitals, homecare, telehealth, health insurance plans, digital engagement platforms, and other services. By tapping into this broad ecosystem, Intermountain has made notable improvements in patient health and become the leading health care system for the people it serves.
No ecosystem, of course, can be built in one fell swoop. It is an incremental process that takes time. To get off on the right foot, organizations should first prioritize a specific pain point that they wish to address and develop a solution to address it. They can then expand their focus to related pain points and add partnerships where needed.
Now more than ever, players have a unique opportunity to use data and technology to optimize the patient journey and radically improve health outcomes. To deliver on this promise, forging the right connections and partnerships will be essential every step of the way. Companies that develop this capability will be best positioned to deliver superior outcomes at scale.