Digital solutions hold extraordinary promise to improve patient care, decrease costs, and reduce waste in the health care system—but they aren’t yet reaching their full potential. Given that 20% to 40% of health care spending is categorized as waste, this is a massive lost opportunity.
So why is digital health falling short of expectations? Based on our analysis, it’s primarily a matter of implementation. Digital solutions cannot deliver well-rounded patient care in isolation, but that’s typically how they are used. To capture their full value, digital approaches must be deployed within a hybrid health care setting that allows patients to seamlessly navigate between virtual and in-person care.
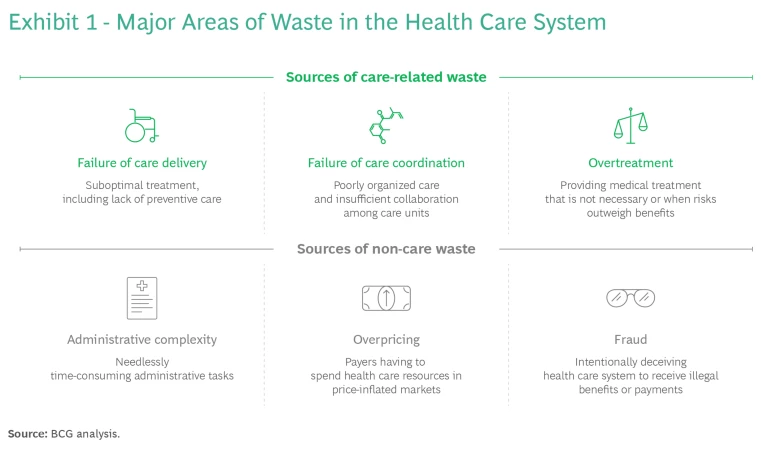
When digital solutions are offered in a hybrid setting, they can significantly reduce three of the largest care-related categories of waste: failure to deliver optimal care, failure to coordinate care, and overtreatment. (See Exhibit 1.) To demonstrate the benefits of hybrid care, we examine case studies for two conditions—melanoma and heart failure—highlighting how this approach can boost prevention, improve coordination of care, decrease overtreatment, and reduce hospital admissions, complications, and mortality. We also identify six enablers necessary to achieve the full benefits of integrated care.
Improving Outcomes with Hybrid Pathways
The pandemic greatly accelerated the transition to digital in health care. In the UK, for example, virtual consultations with general practitioners increased from 3.5% in April 2019 to 40% to 50% between April and November 2020. During this time, home telemonitoring solutions for chronic diseases such as diabetes, COPD, and chronic heart failure—as well as patient self-diagnosis tools such as online symptom-checkers—gained widespread acceptance. Still, most of these solutions only addressed isolated points within the patient journey.
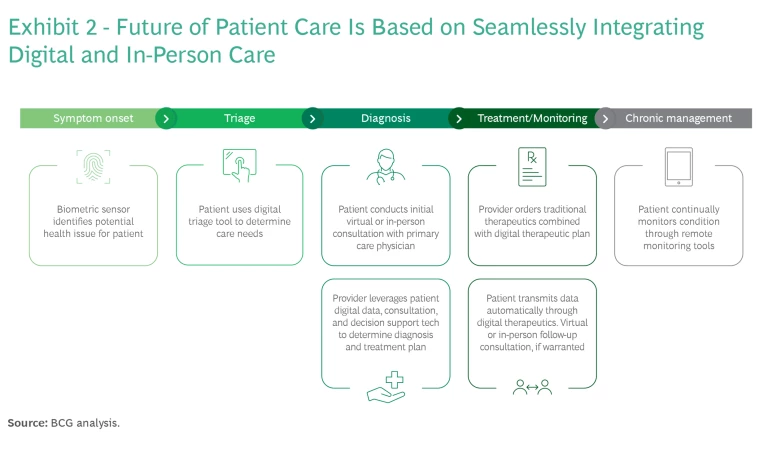
To realize the vast potential of digital in health care, we need ecosystems that integrate digital solutions into the traditional care setting, enabling end-to-end patient journeys. (See Exhibit 2.) Telemedicine providers and other tech companies have a clear head start given their technological capabilities. If they can partner with physical providers and integrate with health care systems to build a hybrid ecosystem, they can deliver more sustainable and valuable business models.
A hybrid approach works well regardless of a health system’s maturity, location, or type of care. It can deliver powerful results in both highly developed and less developed systems as well as public and private organizations. Here are some organizations that have begun to build ecosystems combining digital and physical care:
- Schön Klinik, a group of clinics in Germany, uses hybrid pathways to improve clinical outcomes for patients with mental health issues. They have both inpatient and outpatient settings, and in-person care is combined with digital services to create a seamless hybrid journey for the patient. For example, they developed the “MindDoc” app that assists patients in detecting mental health issues, monitoring symptoms, and learning new coping strategies—and enables self-help through disorder-specific and evidence-based courses and exercises. More than three million people have downloaded the app, and it has been shown to improve symptoms of common disorders like anxiety and depression while decreasing in-person health care utilization. In addition, Schön Klinik offers video-based psychotherapy where patients have weekly interactions with therapists, complemented by activities and courses that are completed individually.
- Kry, a digital health care company based in Sweden, started out as a pure digital health player offering video-based appointments. Through its app, Kry connects patients to a doctor, nurse, or psychologist within minutes, helping patients get a faster diagnosis, prescription, or referral. Kry has since moved into a hybrid care model, establishing partnerships with in-person provider groups and building its own network of physical health clinics. Drawing upon Kry’s network of clinicians, the provider triages the patient to the most resource-efficient level of care directly, whether online or in person. Having delivered more than seven million patient appointments across Europe, Kry is now launching personalized support for patients with chronic diseases such as COPD, asthma, and obesity, underpinned by digital tools.
- GluCare, an end-to-end hybrid diabetes platform based in the United Arab Emirates, pairs in-clinic and virtual care for more efficient management of the disease. Patients are first seen physically by an integrated care team, then continuously monitored digitally, getting nudges to change behavior and improve health between quarterly patient visits. Data from remote monitoring devices are collected and analyzed to provide hyperpersonalized instructions for patients, including medication adjustments. After an initial visit, patients interact with their care team, primarily using virtual consultations. The GluCare health model has shown vastly improved outcomes, lowering hemoglobin A1c by 2.14 percentage points in 90 days (on average), compared to no significant improvement under traditional care, allowing patients to achieve glycemic control much more quickly. Research shows that a 1% reduction in A1c can lead to reductions in end-point disease, death, heart attack, and microvascular complications.
A hybrid approach can deliver powerful results in both highly developed and less developed systems as well as public and private organizations.
Deploying Hybrid Care in Melanoma and Heart Failure
To understand the potential of digital solutions to improve patient outcomes and reduce waste, consider the ways a hybrid model could enhance treatment for two diseases: melanoma and heart failure.
Melanoma
Melanoma is the most serious form of skin cancer. Early detection saves lives, yet only 11% of people have their skin checked regularly. In the UK, 10% of melanoma patients are diagnosed with late-stage melanoma every year. While the number of people being screened regularly is too low, a sharp increase in check-ups would come at considerable cost for the health care system.
This is where hybrid pathways come in. Digital tools for early screening allow patients to self-detect melanoma earlier (and with better prognoses)—and they dramatically lower health care costs. In the UK, melanoma affects approximately 15,000 patients per year, and approximately 6,000 are diagnosed later than is optimal. If all patients were treated at stage 1 of the disease, melanoma treatment costs could be reduced by 30% in the UK, saving an estimated €13 million annually.
To support prevention, AI-based, patient-operated tools can be used to send skin-check reminders, allowing patients to examine themselves. If the tool identifies something suspicious, the patient can send images to a provider for follow-up. Lesion-tracking services also assist patients in monitoring and identifying changes in suspicious pigmented lesions (SPLs) over time. In ongoing research at MIT, a lesion-analysis tool achieved more than 90.3% sensitivity in distinguishing SPLs from nonsuspicious lesions—comparable accuracy to expert dermatologists. These tools increase patients’ access to screening services and improve monitoring and early detection of melanoma without burdening the system and contributing to overtreatment.
For practitioners, AI-based tools can support decision-making and decrease screening errors—and at lower costs than non-digital methods. Studies have shown that AI tools improve diagnostic precision in identifying malignant lesions and deliver results in seconds. Digital tools also enable primary care physicians to consult with specialists remotely, via a digital platform, thereby eliminating unnecessary procedures (such as biopsies for harmless lesions). (See Exhibit 3.)
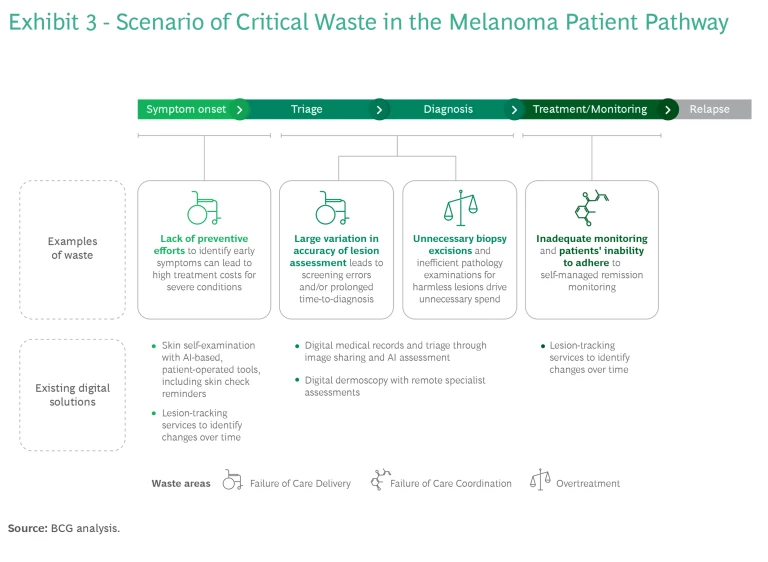
Pilots demonstrating the hybrid model have been conducted in Stockholm County, Sweden, where a digital dermoscopy platform allows specialists to make assessments remotely. Efficiency in melanoma detection is commonly measured by the number of biopsy excisions needed to detect one case of melanoma. By leveraging the dermoscopy platform, one pilot reported the number of biopsy excisions in primary care dropped to just 6, compared to other similar care units reporting between 15 and 30. In another pilot, fewer patients required face-to-face consultations and instead received an assessment remotely, resulting in more than 35% in cost savings on diagnostic efforts for melanoma.
In the UK, more than 90% of biopsies do not detect melanoma, and reducing the number of excisions to levels in the Sweden pilot could reduce costs by €55 million annually. Beyond reducing costs and waste, a hybrid care pathway for melanoma significantly improves patient outcomes through earlier detection and intervention.
Heart Failure
In many parts of the world, heart failure is the leading cause of hospitalizations among older adults. A key element of treatment is the prevention of disease progression, which requires regular monitoring of patients and adaptations to their medication regimen.
The main area of waste in heart failure care lies in preventable exacerbations; that is, patients who aren’t properly monitored can end up with acute heart failure. Reducing the number of patients who advance to an acute condition has significant impact on treatment outcomes. In the UK, remote monitoring can reduce heart failure exacerbations by 21%, affecting 15,000 people and reducing costs by €42 million (approximately 8%) per year.
For patients with early symptoms of heart failure, it’s important to have access to comprehensive medical records documenting any prior disease, symptoms, and family history. Medical devices and technology must also track the patient journey through the hospital and beyond, following them across settings, specialists, and circumstances. Digital solutions that directly integrate into the patient’s medical records can significantly speed up time to diagnosis and treatment, while reducing costs.
Once treatment begins, many digital solutions that support coordinated care are readily available and easy to adopt, lowering barriers for patients to contact their physicians and enabling continuous rather than sporadic monitoring. Telehealth platforms that offer remote video consultation—particularly for patients at risk of relapse—provide a combination of continuous monitoring and improved communication among various providers that can alleviate pressure on the health care system by replacing inefficient consultations, thereby lowering costs and improving outcomes. (See Exhibit 4.)
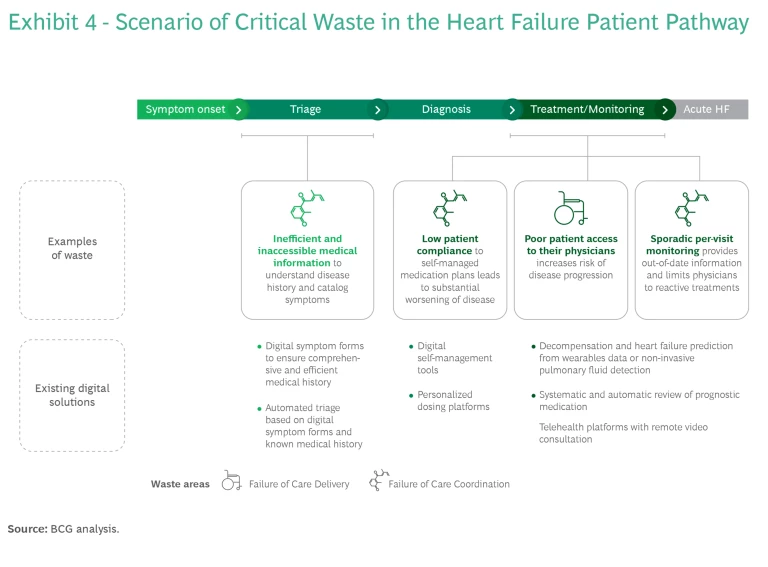
In preventing exacerbations, digital tools can provide significant value for monitoring patients’ conditions and medications, predicting decompensation, and enabling timely intervention. Wearables can track physical activity, heart rate variability, EKG, oxygen levels, and blood pressure—and all of this data can be instantly communicated to the patient’s physician team. In a UK-based meta-analysis, remote monitoring of heart failure patients through structured telephone support and data from consumer devices reduced exacerbations by 21% and decreased all-cause mortality by 20%.
Core Enablers for Digital–Physical Patient Care
Based on BCG’s experience, we have identified six key enablers for successfully implementing hybrid care pathways at scale.
Demonstrate a clear value proposition for patients, providers, and payers.
Organizations need a strong business case that clearly improves care outcomes, avoids unnecessary examinations or admissions, and prevents the progression of disease. The business case must also deliver clear savings for payers and for the health care system.
Build the ecosystem.
Implementing hybrid pathways will require significant upfront investment to build a platform that connects providers, payers, suppliers (pharmaceutical companies, medtech, pharmacies, and others), and digital companies. All of these partners deliver complementary offerings that must be coordinated to provide coherent diagnostic, therapeutic, or care solutions for patients. Players should analyze existing gaps and prioritize patient pathways that will deliver the best results from combining digital and in-person care.
Create incentives for participation in the ecosystem.
Stakeholders need strong incentives to join hybrid ecosystems, and not just financial incentives. All participants should share the benefits. Organizations need to construct fair reimbursement mechanisms for digital services such as home monitoring and digital therapeutics, ensuring adequate remuneration.
When digital solutions are blended into hybrid, end-to-end patient journeys, the benefits for the health care system—and the patient—are amplified.
Make digital solutions easy to use.
To maximize adoption of digital solutions, the technology must be user friendly. A study of mobile health apps shows that the user experience and user interface (UX/UI) are directly related to user satisfaction. A solution with a poor UX/UI runs a high risk that users will abandon the tool—and warn others of its flaws. To prevent this, patients must be at the center of the design process. This is especially important for medical conditions like diabetes and heart failure because digital solutions address a broad spectrum of users in different age groups with different digital affinities. Special training that introduces people to digital solutions and how to use them can increase their adoption.
Improve data infrastructure and interoperability.
To create a hybrid model that merges in-person and virtual care, health care professionals and patients must have immediate, automated access to electronic health records, regardless of location, with patient consent and in accordance with privacy regulations. Interoperable systems that communicate with each other within and across health care systems can improve the quality of treatment, streamline care, and reduce costs.
Support regulatory change.
Regulators have a key role to play by establishing the necessary frameworks that foster cooperation among payers, providers, and suppliers. Health care organizations can encourage regulators to support innovation that enables hybrid ecosystems and advocate for regulatory policies that promote data sharing, while ensuring data security.
Moving forward, health care CEOs should be thinking about ways hybrid pathways can reduce waste and improve outcomes within their unique context. Here are three key questions to get started:
- What are the biggest areas of waste within my organization—and how are we using digital solutions to address these today?
- How can hybrid solutions help to reduce waste even more?
- How can my organization implement hybrid pathways to achieve near-term impact and fund the journey?
When digital solutions are blended into hybrid, end-to-end patient journeys, allowing patients to seamlessly navigate between virtual and physical care settings, the benefits for the health care system—and the patient—are amplified. By embracing this approach, and implementing the six enablers, health care organizations can significantly reduce waste and improve outcomes.






