Globally, rehabilitation and compensation schemes that care for victims of accidents and injuries are under mounting pressure as the costs of care continue to outpace broader economic growth. Medical cost inflation is running at over 6% per annum, partially due to health care sector wages increasing at 5%. At the same time, compensation costs are increasing as recovery periods extend due to both aging workforces and the growing incidence of psychological injuries, which now represent 24% of claims across Australia. Consequently, local schemes such as WorkSafe Victoria and iCare are grappling with substantial financial challenges, with deficits of $1.6 billion and $660 million respectively.
To address these pressures, leading global rehabilitation and compensation organisations are starting to embrace a value-based approach to cost and outcomes management. Instead of simply reimbursing costs for health care and lost wages, they are working to maximise client outcomes relative to costs by actively managing clients’ end-to-end rehabilitation journeys from lodgment to treatment, to recovery.
Implementing Value-Based Solutions to Manage Cost Pressures
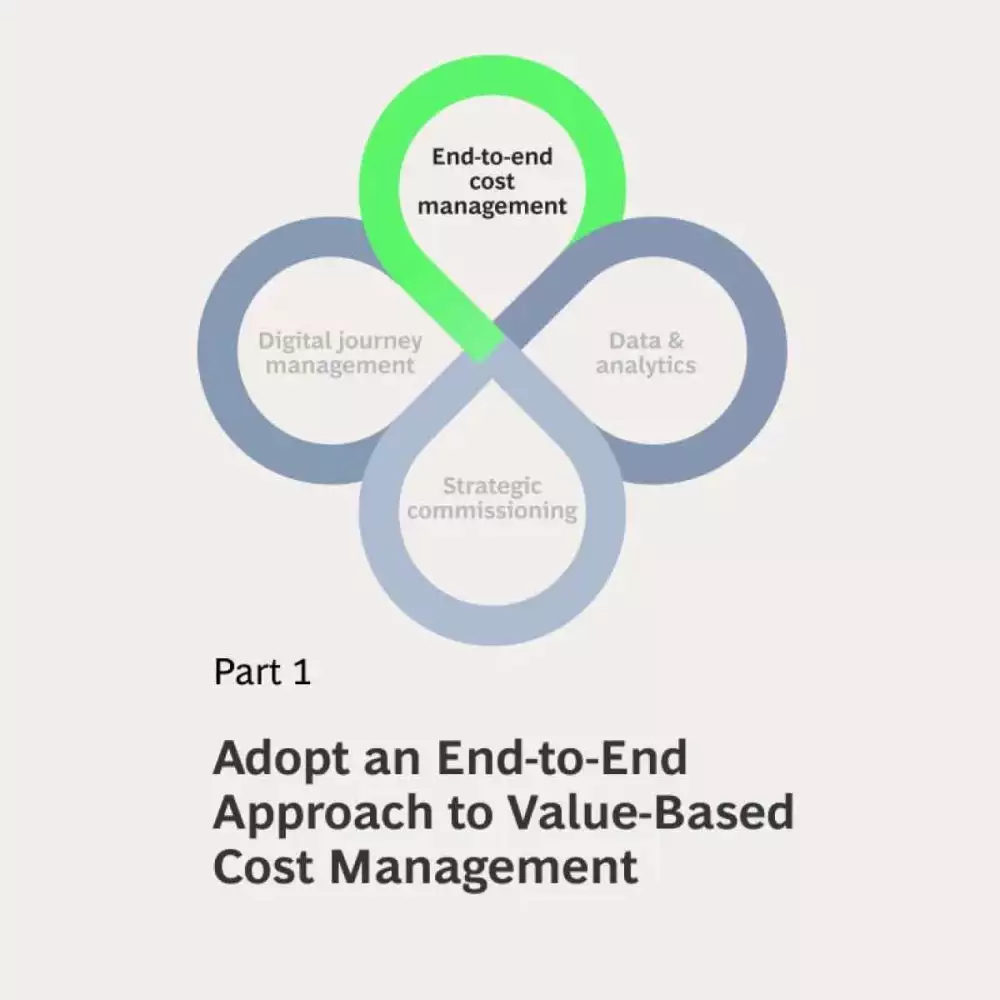
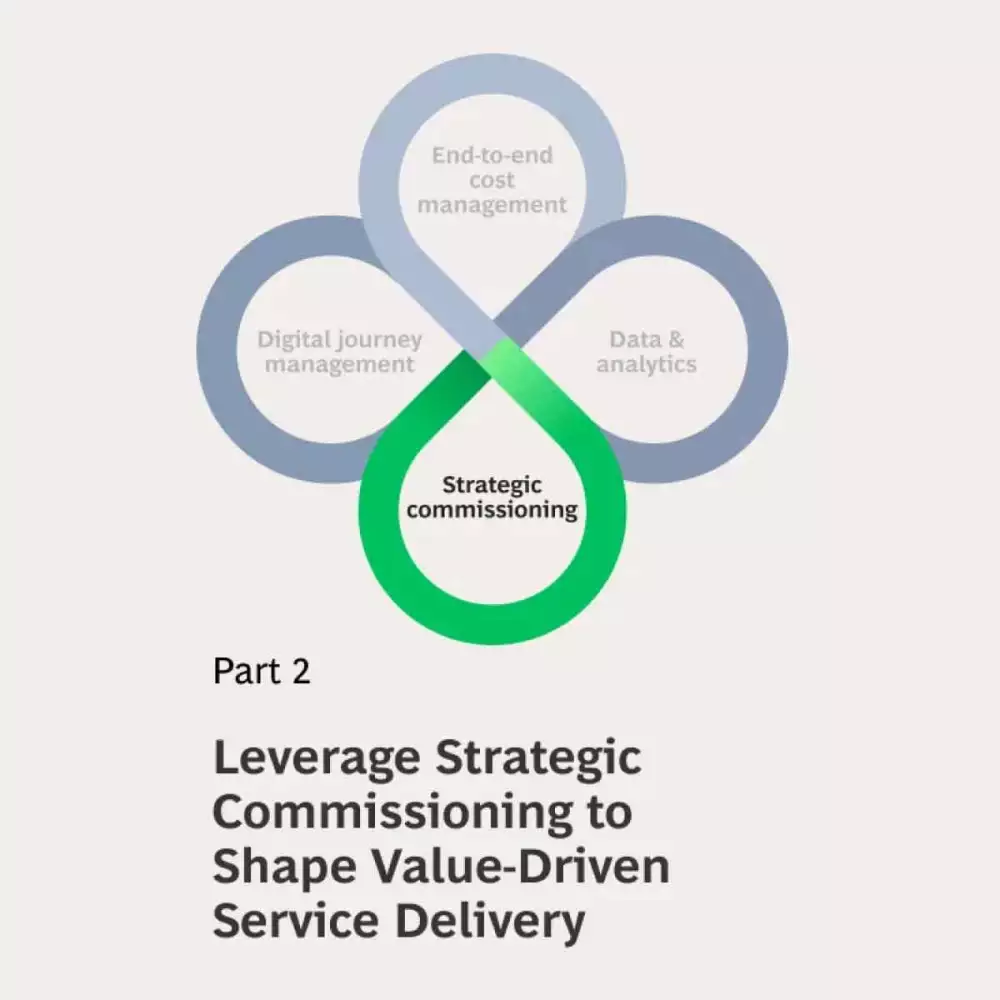
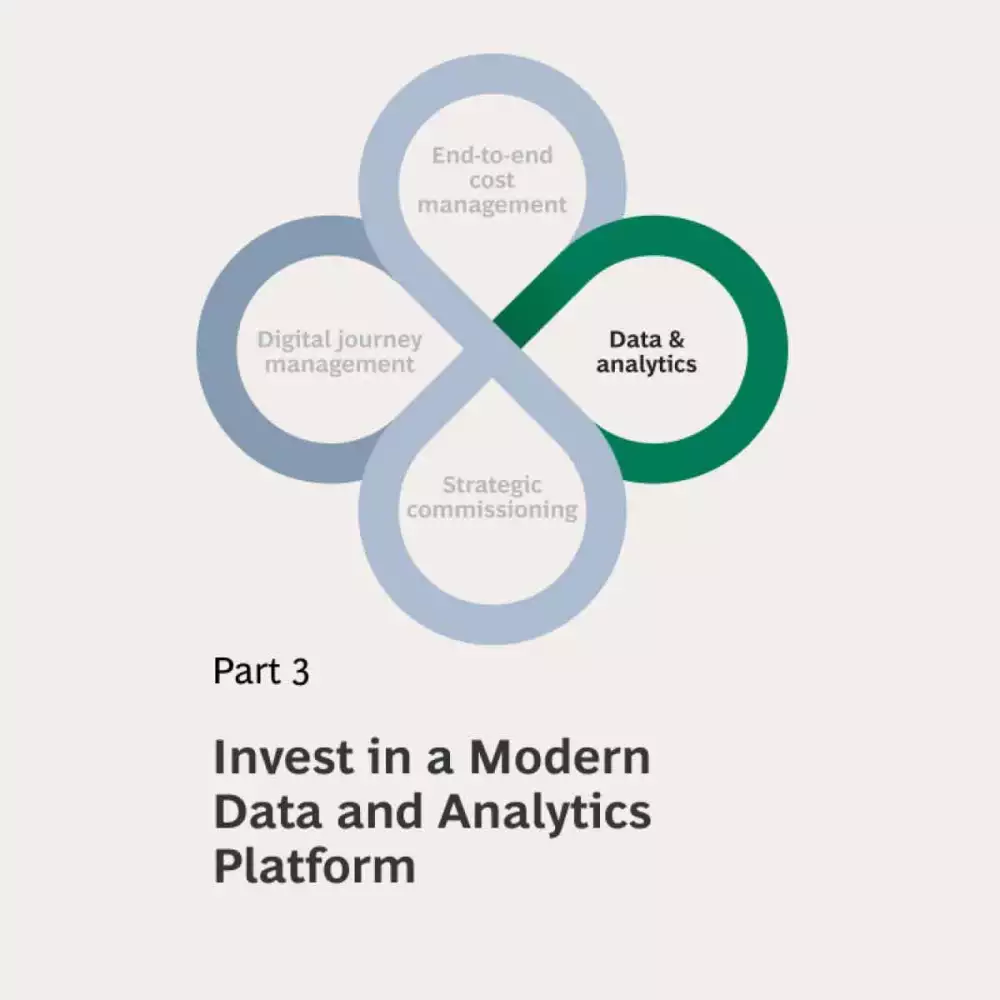
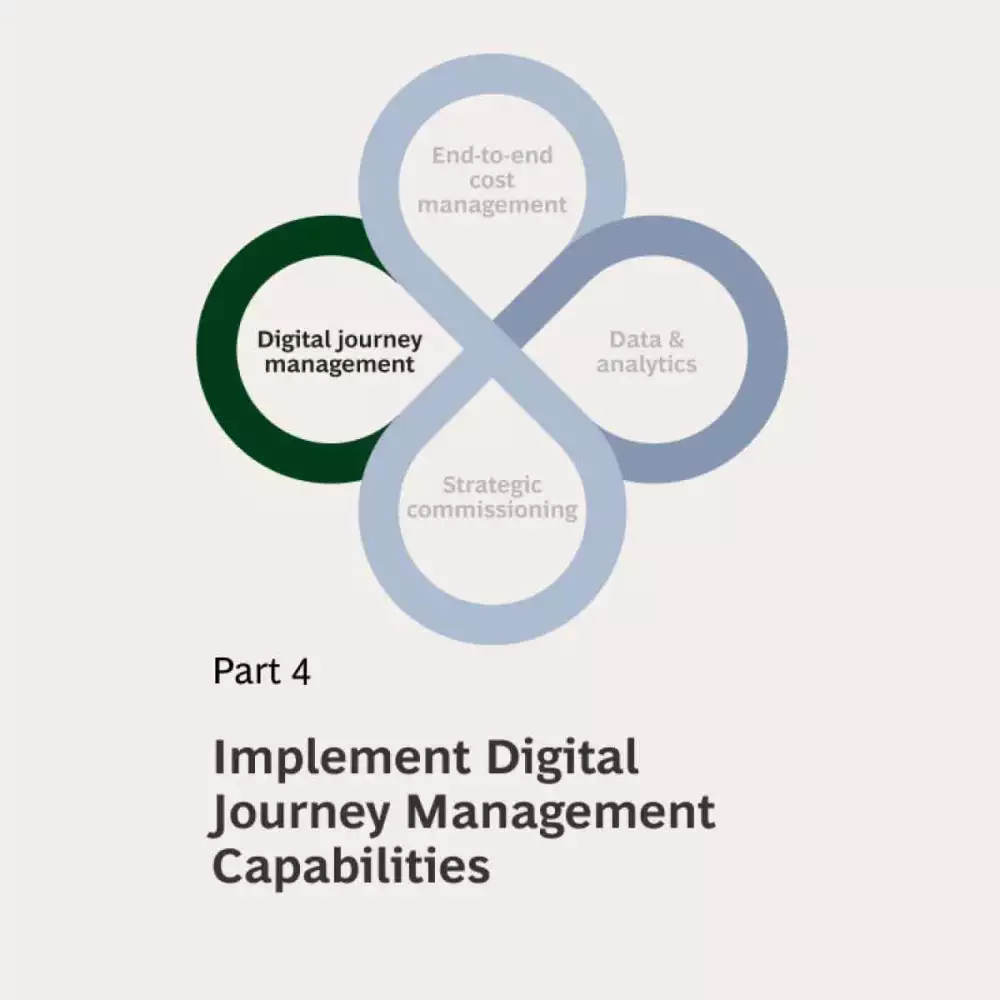
Exhibit 1: Four pillars of value-based care are helping rehabilitation and compensation agencies manage end-to-end cost pressures
Rehabilitation and compensation agencies that are implementing value-based cost and outcomes management typically adopt four key approaches:
Shift to managing end-to-end costs and outcomes
Historically, costs and outcomes have tended to be managed in categories related to individual steps in the care journey. For example, surgical costs and outcomes have typically been managed quite separately to rehabilitation costs and return to work services. By shifting to end-to-end measurement and analysis of different client journeys, rehabilitation and compensation agencies can assess the drivers of variation in cost and outcomes. This allows organisations to understand the drivers of total costs and outcomes for different types of injury (e.g. repetitive strain injuries vs. limb fractures vs. concussions) and different client segments (e.g. younger sedentary workers vs older manual workers). These insights can inform decisions to focus effort on renegotiating unit costs, managing provider variation or improved internal management of control points along the journey (e.g., approvals of service, extensions of support, redirection into more intensive management).A rehabilitation and compensation agency facing sharply rising costs in step-down care adopted BCG’s value-based approach. To gain an end-to-end understanding of the cost drivers, we conducted an in-depth analysis of discharge patterns from hospitals, including factors such as bed availability, discharge planning variation, and average length of stay. We also examined geographic and ethnic disparities in access, along with the factors contributing to extended stays in step-down care and variations in daily costs. By uncovering these end-to-end cost dynamics, we were able to recommend targeted process improvements to better align outcomes and costs, enabling more efficient management of the rehabilitation journey.
Leverage strategic commissioning to shape a value-driven market
Rehabilitation and compensation agencies often think of themselves as price takers in large health care service markets. The reality is often far more nuanced, with many compensation agencies playing significant roles in specific care niches and constituting a significant component of some providers’ incomes. In addition, other personal service markets (e.g. personal attendant care, home modifications and transport services) have been radically disrupted by on-line market platforms, but compensation agencies have continued to procure these services using panel provider arrangements, often with high costs to arrange specific work orders. Many agencies are now beginning to experiment with new forms of contracting and commissioning to reshape service delivery markets and increase focus on outcomes.BCG collaborated with an agency to develop their strategic commissioning capabilities, starting by testing two distinct markets for value creation opportunities. In the first market, we highlighted the potential given to drive down unit costs by offering long-term contracts for all or a significant portion of volume in a local market. While our client was not the largest single payer in the market, consolidating their volumes would offer a significant utilisation benefit and the multi-year guarantees would reduce provider risk, allowing further investment in capacity. In the second market we identified that consolidated purchasing could unlock value by leveraging commitment to improved care models—focused on better screening against surgical eligibility criteria, faster access to surgery where indicated, and a greater focus on post-surgical outcomes. This approach underscored a critical insight: by deeply understanding market structures, agencies can target their strategic commissioning to deliver value across the system.
Invest in a modern data and analytics platform
Value-based approaches rely on the ability to connect data along the client journey. This client centric perspective allows an understanding of how variation in treatment management corresponds to variation in outcomes. Modern data and analytics platforms enable this analysis and support tracking of variation across clients and providers and supports identification of opportunities to more tightly define treatment pathways and requirements. Sharing data with providers on metrics such as claim processing times, time to surgery, readmission rates, return to work timing and reinjury rates helps drive ongoing improvement.One health care payer was unable to make data-driven decisions due to its limited understanding of data, a legacy system that limited access to what low quality data they had, and few analytical tools. Together, we identified and prioritised 100+ data and analytics use cases across the business with the potential to generate $10-20 million in cost savings and $20-30 million in revenue uplift with only the top 16 use cases. By organising the data flows and integrating the available data into claims management decisions, agencies can intervene as unwarranted variation is identified.
Implement digital journey management capabilities
Treatment approvals can be a time-consuming and frustrating process for both providers and clients. But poorly managed approvals processes can lead to inappropriate approvals and a proliferation of treatment models with limited evidence or benefit. A user-friendly digital journey platform connects clients and providers to streamline claims management and improve outcomes. It helps compensation agencies capture consistent cost and outcome data that can help them gain a deeper understanding of client needs and respond dynamically. It allows compensation agencies to improve resource allocation and provide real-time support to clients throughout their treatment and rehabilitation journeys.An integrated health care system engaged BCG to design, build and run a patient portal that oversees every element of the health care journey. We worked with multidisciplinary teams and tested the platform with users to launch a responsive website and iOS/Android app that provided wide access to timely and appropriate information and care. In parallel, we built the system’s capabilities to monitor and manage the platform following our engagement.
Making the Transition to Value-Based Care
While the path forward is clear, the challenge often lies in execution. Transforming rehabilitation and compensation agencies requires striking a delicate balance—delivering immediate results while also building sustainable, long-term frameworks. Legacy processes and systems often complicate this effort, and organisations can easily fall into the trap of chasing the ‘perfect design’ at the expense of practical, short-term wins. To overcome these challenges, we recommend 4 practical steps that can deliver rapid and sustainable results:
- Focus on a small number of key journeys to build an end-to-end cost view
Focusing on a specific client group enables organisations to develop more precise, tailored solutions. Start with the data and insights already available, even if it requires some laborious efforts to create a one-off data set. Then combine this with qualitative research to map out the client journey from diagnosis to recovery. By identifying key interactions and touchpoints, organisations can make informed trade-offs that reduce long-term costs. For one client, the potential savings from reducing unit costs of a particular surgery to benchmark levels were completely dwarfed by the potential impact of reducing variation in return-to-work timing which accounted for more than 50% of the end-to-end costs. - Empower teams using a test-and-learn approach
Empower integrated teams comprised of frontline claims managers, procurement staff, provider engagement leads and clinical advisers with the authority, autonomy and resources to experiment with end-to-end cost and outcome improvements within a specific segment. By involving frontline teams in solution design and testing, organisations can uncover inefficiencies not immediately evident in datasets—such as duplicate referrals or conflicting information—that impact decision accuracy and costs. Leadership and these integrated teams should embrace a culture of rapid iteration and learning. While not every change will yield immediate gains, each test deepens an agency’s understanding of cost drivers. For one compensation agency, BCG facilitated a rapid, data-driven idea generation process and then prioritized a small number of initiatives to test. Fortnightly reviews were then used to monitor impact and decide how to refine the approach to ensure best return-on-investment. Within only 14 weeks, two teams identified and trialed 10 initiatives and signed off a plan for full implementation with senior management, with a target impact of $45M in year savings. Engage providers collaboratively
Rehabilitation and compensation organisations often limit the effectiveness of their market intelligence gathering out of concern for probity in their procurement processes. Agencies should work with their probity advisers to find way to engage much more deeply with providers to understand perspectives on how to better deliver on their objectives. One effective approach is using a Request for Information (RFI) to gather insights and options before approaching the market with specific requirements or specifications. Other organisations have structured ways to take “market soundings. ” It is important to engage with a diverse range of providers rather than working only through peak bodies as this allows agencies to tap into the diversity of views and ambitions within each sector.In BCG’s experience , the greatest challenge in shifting towards paying for value involves aligning with providers, but deep engagement can reveal opportunities for innovation and impact.
- Invest in capability to supercharge change
Rehabilitation and compensation agencies must build their own capabilities to effectively manage costs and outcomes together. However, partnering with external experts can help teams deliver impact faster, provide fresh perspectives and accelerate the process of capability development. In our experience, organisations that collaborate with external partners achieve faster, more sustainable results while equipping their teams with the skills needed to independently address future challenges. In recent projects, we’ve trained teams in our value-based approach to cost management, enabling them to apply these principles on an ongoing basis. By capturing the approach in a playbook, we ensure consistent use across the organisation. This collaborative model positions agencies to drive their own success and meet evolving challenges with confidence.
Value-based approaches to cost and outcomes management are helping rehabilitation and compensation organisations manage costs and improve outcomes in the face of growing medical costs and other ongoing challenges. Shifting to this approach requires organisations to shift to a focus on end-to-end journeys, empower teams to innovate, and leverage data-driven insights. Partnering with experienced advisors can also accelerate change and build long-term capability to reduce costs and improve outcomes.
BCG has the proven experience and tools to help rehabilitation and compensation agencies navigate the complex shift to value-based care, ensuring sustainable results. Contact us to find out more about how we can partner to unlock innovation, build internal capability, and deliver better outcomes for your clients and stakeholders.