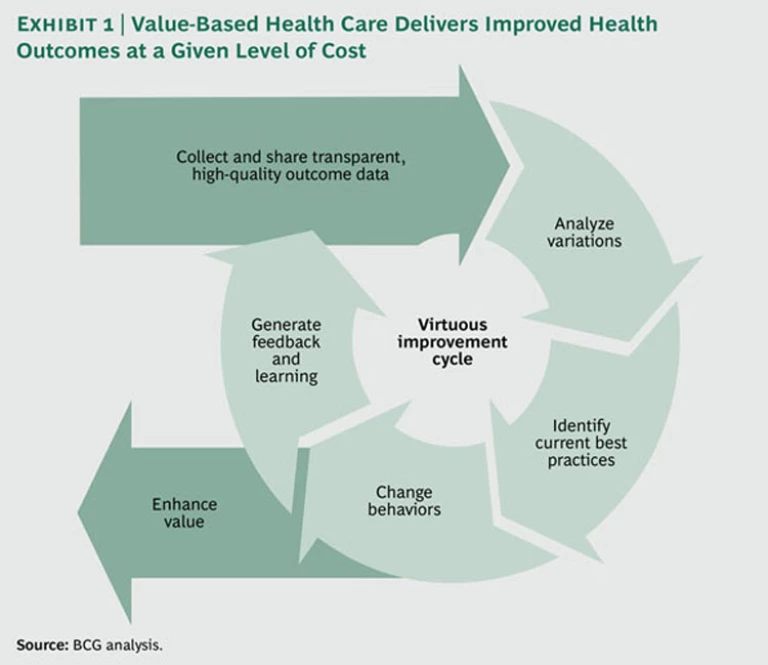
In the global struggle to manage the cost of health care, both clinicians and policy makers are increasing their focus on value . Health systems around the world are starting to document variations in health outcomes and, at times, remarkable differences in clinical practice. Making the data available allows clinicians to identify best practices and helps steer resources toward the clinical centers and specific clinical interventions that achieve the best results. Such efforts are facilitated by the proliferation of new systems and capabilities in health care informatics that make it possible to collect outcome data and share the information broadly with clinicians and the public. We call such efforts to improve health outcomes—while also maintaining or lowering costs— value-based health care . (See Exhibit 1.)
Value-based health care is becoming the focus of many health-care-reform efforts around the world because it promises to be a more effective and more sustainable approach for limiting the increase in health care costs than traditional approaches such as utilization reviews or cost controls. The Boston Consulting Group has recently developed a methodology—a maturity assessment framework—for assessing the progress of a country’s health system in adopting and institutionalizing value-based health care. In 2011, we used this framework to evaluate the health systems of 12 countries: Australia, Austria, Canada, Germany, Hungary, Japan, the Netherlands, New Zealand, Singapore, Sweden, the U.K., and the U.S. (In the course of 2012, we will be adding other countries to the list.)
Our research shows that a number of countries have begun to build the infrastructure and processes to support a value-based approach, but some countries are significantly farther along the learning curve than others. Despite this differential in development and major differences in the structure and organization of national health-care systems, however, there is much to learn from each country.
In this report, we describe our approach for assessing a country’s progress toward value-based health care; identify some best practices that are emerging, as well as some common issues that countries face; and discuss what governments, in particular, need to do to support value-based health care.
The Maturity Assessment Framework
As part of BCG’s extensive work in the field of value-based health care, we have identified key success factors for the effective implementation of a value-based approach. (See “BCG and Value-Based Health Care.”)
BCG and Value-Based Health Care
Since 2009, The Boston Consulting Group has conducted extensive research in the field of value-based health care, an approach to improving health care management that emphasizes maximizing value, defined as patient outcomes divided by costs.
We started this research in 2009, when a group of senior health-care leaders in Sweden asked BCG to analyze that country’s disease registries and evaluate the opportunities and costs involved in expanding the registry model to include other conditions. Our study concluded that with an annual investment of $70 million in disease registries, data analysis resources, and IT infrastructure, Sweden could reduce its annual growth in health care spending from an estimated 4.7 percent to 4.1 percent. The estimated cumulative return over ten years would total more than $7 billion in reduced direct health-care costs.
Encouraged by the initial results of the Swedish study, BCG expanded its research in 2010, analyzing the impact of disease registries in other countries. In 2011, we published the results of an international study of 13 registries in five countries and across six major disease areas. Our research, which has been featured in Health Affairs, demonstrated that disease registries can be used not only to improve the quality of care and health outcomes but also to lower total health-care costs for a given condition.
In addition to the maturity assessment framework described in this report, BCG research in value-based health care has also looked at the competitive impact of the trend on the pharmaceutical sector and the requirements for constructing robust health-outcome databases.
- Clinician Engagement. The cornerstone of value-based health care is broad and active engagement on the part of the clinical community. For example, our international study of 13 disease registries in five countries revealed that the improvement in health outcomes is greatest when clinicians themselves are responsible both for collecting and interpreting data and for leading efforts aimed at clinical improvement.
- National Infrastructure. Clinician engagement can be greatly facilitated and supported by the existence of common standards for tracking diagnoses, treatments, outcomes, and costs at the patient level; a limited number of shared IT platforms; and a common legal framework regulating the use of patient data.
- High-Quality Data. Value-based health care is a data-driven approach for improving the quality of care. The most effective way to collect relevant data is through disease registries that track selected health outcomes in a population of patients with the same diagnosis or who have undergone the same medical procedure. The systematic analysis of outcome data from a broad range of clinical centers allows providers and payers to identify, codify, and promote treatment protocols that have proved to yield better, more cost-effective care.
- Outcome-Based Incentives. Value-based health care requires not just the comprehensive collection of outcome data but also their active dissemination and use. The fourth success factor is the use of outcome data to realign incentives in the health system so that stakeholders are encouraged to optimize health value. When such incentives are in place, the system itself drives changes in the ways clinicians practice, payers reimburse, and suppliers of drugs and medical devices develop and deliver products and services.
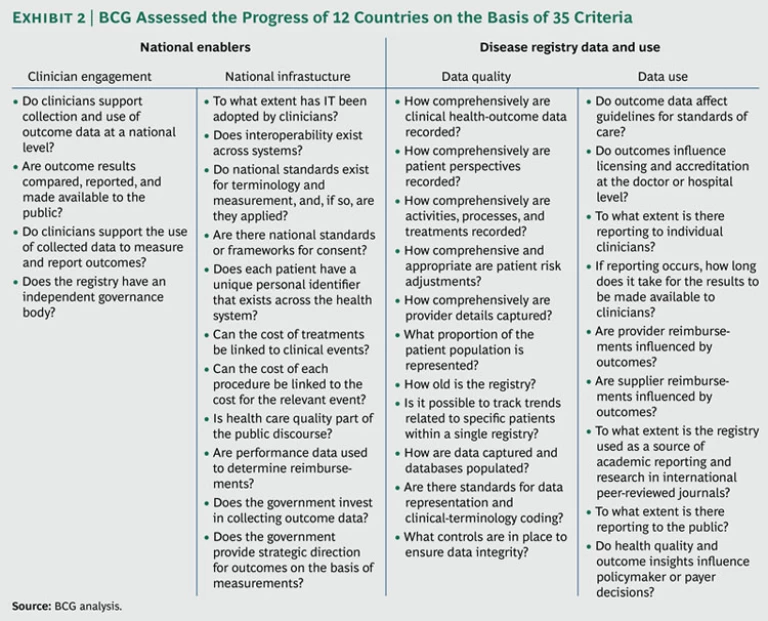
The BCG maturity-assessment framework uses these four success factors to evaluate a country’s progress toward value-based health care on two broad dimensions. It combines a top-down assessment of national enablers of value-based health care (clinician engagement and national infrastructure) with a bottom-up assessment of data quality and use at existing disease registries across 12 major health conditions. We have defined 35 specific criteria—15 at the national level and 20 at the level of individual disease registries—that are essential for establishing an effective value-based system. (See Exhibit 2.) A country’s performance on each criterion is rated on a scale of 1 to 5, with 1 representing low readiness and 5 representing best practices. (The framework was developed on the basis of previous BCG research in the field, a comprehensive survey of the medical literature, and 139 interviews with representatives of national health departments and with international health-outcome experts.)
Assessing National Enablers. At the national level, the framework attempts to answer two key questions:
- To what degree are a country’s clinicians, government officials, and health-care policymakers committed to creating and using a system of high-quality health data?
- To what extent is a national legal and IT infrastructure in place for collecting health outcome data and linking those data to issues of cost?
For example, to assess the degree of clinician engagement, we ask: Do clinicians support collection and use of outcome data at a national level? Are outcome results compared, reported, and made available to the public in a useful form? Is there support for using performance data on outcomes to determine reimbursements?
To assess the extent to which a country has in place a national legal and information infrastructure that allows the comprehensive collection and sharing of health outcome data, we ask: Do national standards exist for outcome metrics (and, if so, are they actually applied)? Does each patient have a unique personal identifier that can be used across the entire health-care system? Is there a national framework governing consent for the use of health information? To what extent has IT (including electronic health records) been adopted by clinicians and become part of normal clinical practice? How interoperable are existing IT systems and data sets? Can the cost of a given treatment be linked to each clinical event recorded in an outcome database?
Assessing Disease Registry Data and Use. Ideally, a disease registry is simultaneously a repository of data that are useful in outcome research and an important institutional catalyst for efforts to improve health outcomes over time. By identifying variations in outcomes within the same population, registries make it possible to benchmark and assess comparative performance at the clinic, regional, national, and even international level. In-depth analysis of the causes behind variations in performance can lead to the identification of best practices. Active dissemination of those best practices and support for enabling their adoption reduce variations in clinical practice and improve outcomes.
Our framework evaluates data collection and use at a country’s disease registries across a broad range of health conditions: two acute conditions (acute myocardial infarction and stroke), three chronic conditions (chronic renal failure, diabetes, and schizophrenia), four surgical procedures (cataract surgery, spinal surgery, and hip and knee replacement), and three forms of cancer (breast cancer, cancers of the digestive tract, and hematological cancers such as leukemia and lymphoma). These conditions, which are among the most common causes of avoidable morbidity and mortality in the developed world, represent approximately 30 percent of disability-adjusted life years lost. We assessed the adequacy of the data collected by a country’s disease registries along three critical dimensions:
- The number of data variables collected for each individual case—including clinical outcomes, patient-reported metrics, descriptions of the nature and process of treatment given (for instance, the type of prosthesis or length of hospital stay), risk adjustment data, provider details, and cost data
- The number of observations across the entire population for a given condition—for example, the percentage of patients covered, how long a repository has been in use, and the longitudinal nature of the data
- The degree of quality control as represented by methods of data capture, usage standards, the process for validating data and ensuring its integrity, and whether or not there is a formal governance body regulating the registry
In addition to evaluating the databases themselves, the framework also assesses the extent to which the data are used to drive clinical practice and health policy and to align incentives around value across the health care system. For example, to what extent does reporting to individual physicians take place? Do outcome data direct the development of guidelines for patient care or influence licensing and accreditation at the level of the hospital or the individual physician? Are data released to the public? Are observational data used in the ongoing monitoring of new drugs and medical devices after they have been launched? Do outcomes influence reimbursement?
Country Findings
To assess each country’s progress on the two dimensions described above, local BCG teams reviewed available documented data on the national health system and the dominant registry for each of the 12 target conditions—annual reports, published academic papers, and, in many cases, internal reports provided by the registry administrators. The teams used a standardized set of descriptions to assign a numerical score—from 1 through 5—for each of the 35 assessment criteria. The scores for all 12 countries were reviewed for consistency by a global project manager and then presented for feedback to at least one topic expert per registry in each country. These external reviewers used the same criteria and grading system.
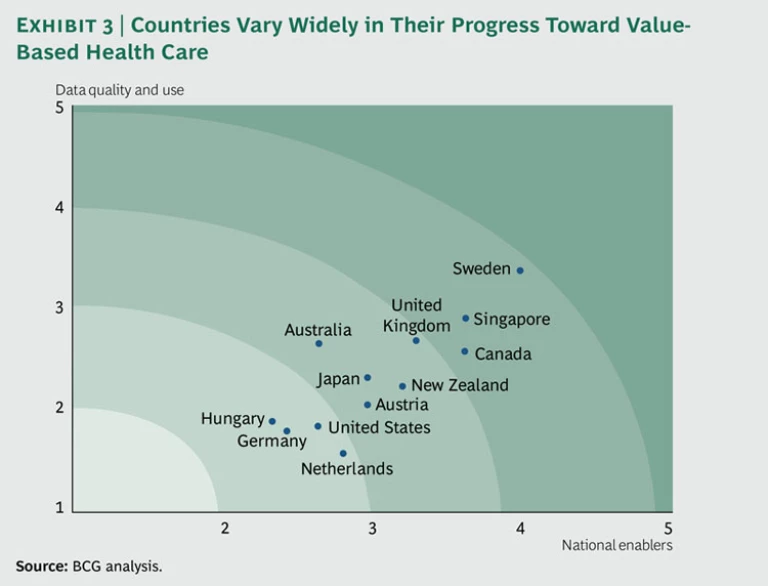
Exhibit 3 ranks the 12 countries in our sample on the two broad dimensions of our framework: national enablers and the quality and use of disease registry data. As the exhibit illustrates, when it comes to implementing value-based health care, Sweden is the most advanced country on our list, followed closely by Singapore. Germany and Hungary have the furthest to go.
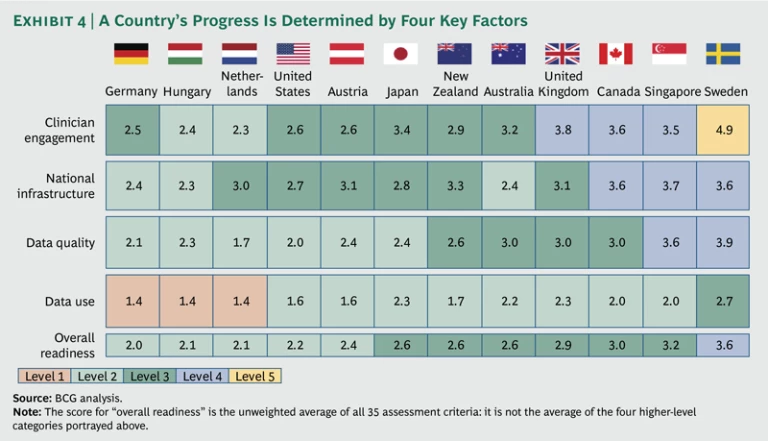
Exhibit 4 displays the average score in the four broad categories that track our success factors, as well as a score for overall readiness, which is the unweighted average of all 35 criteria. In this approach, Germany is at the bottom of the list, owing mainly to limited access to high-quality data and poor data utilization.
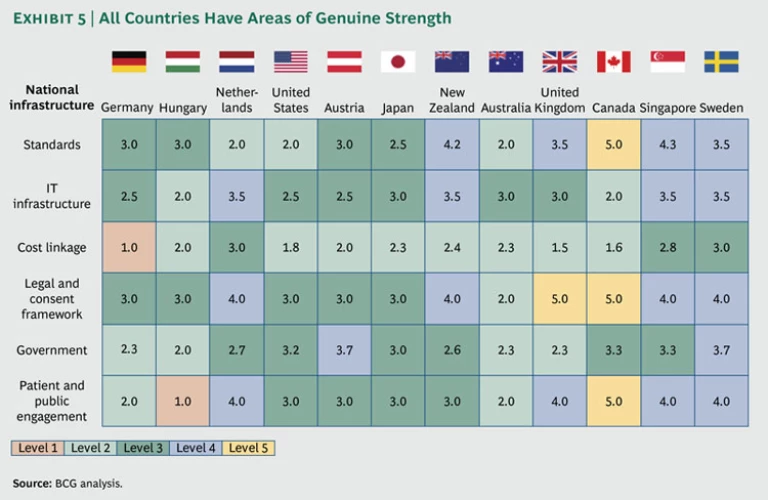
It is important to emphasize, however, that even those countries in our assessment with low average scores have some areas of genuine strength. Exhibit 5 disaggregates the scores of the 12 countries in the national-infrastructure category. It shows that the Netherlands, one of our ranking’s low overall performers, has quite a strong legal and consent framework, as well as a high-quality IT infrastructure and relatively engaged population.
Our assessment also suggests that there are some common steps on the road to value-based health care—critical phases with their own special challenges and opportunities.
Getting Started. Some countries are just starting to implement a value-based system. Although they have some promising value-based initiatives, they are still largely preoccupied with managing the traditional care model.
Hungary is a good example. Like all the other countries we studied, Hungary has some strong points. For example, the Hungarian Pediatric Cancer Registry has been an active participant in the development of common metrics and a common data-collection platform, both in Europe and internationally, and has been a leader in getting Hungarian pediatricians to follow international protocols for the treatment of pediatric cancers. And yet, the registry remains a relatively isolated pocket of best practice in a country with few registries, low adoption of IT on the part of clinicians, and little government encouragement for value-based health care. Given this starting position, the best approach for Hungarian clinicians hoping to build engagement around a value-based approach is to draw on the considerable international disease-registry experience to further develop the Hungarian registry network.
The Netherlands is another country still very much in the starting phase of value-based health care. In 2007, the Dutch government took the lead by bringing together major stakeholders in the health system—including clinicians, patients, hospitals, and health insurers—to launch an initiative that would create outcome transparency in 80 diseases by 2011. Despite significant efforts, however, the initiative foundered on stakeholders’ disagreements about what constituted quality outcomes, ineffective compromises, and insufficient clinician buy-in.
More recently, however, a number of clinician groups in the Netherlands have independently established some excellent registries. The demonstrated successes of these “early adopters” should increase engagement among Dutch clinicians and significantly accelerate progress toward value-based health care.
Going National. In a number of the countries that we studied, considerable progress has been made in the development of excellent disease registries and even in putting some key national enablers in place. For one reason or another, however, progress has been uneven in the country as a whole. The next big challenge—and opportunity—is to expand value-based initiatives to the national level.
This is the case, for instance, in countries that have a relatively fragmented national health-care system. The classic example is the U.S. The country has some excellent disease registries, including, for instance, the Cystic Fibrosis Foundation Patient Registry , the Society for Thoracic Surgeons’ STS National Database , and the American College of Cardiology’s CathPCI Registry . What’s more, some regional health providers such as Kaiser Permanente and Intermountain Healthcare have made considerable progress in tracking outcomes in their own patient populations and in creating incentives for clinicians to use best practices identified through outcome research. (Keep in mind that the 8.9 million patient population covered by the Kaiser Permanente system is roughly equivalent to the total population of Sweden.)
However, the high complexity and extreme fragmentation of the U.S. health system mean that it is difficult to build on these best practices to develop and implement a truly nationwide approach to value-based health care. One dramatic example: The U.S. has no national hip-replacement registry, but Australia, whose population is one-tenth the U.S. population, maintains an excellent national hip-replacement registry. Australia was, therefore, able to identify problems with DePuy’s ARS metal-on-metal implant, warn surgeons not to use the device, and eventually prompt a voluntary recall by its manufacturer from the Australian market in December 2009—a full seven months before the device was recalled by the U.S. Food and Drug Administration in July 2010. (After completing a successful pilot in May 2011, the American Joint Replacement Registry , an initiative of the American Academy of Orthopaedic Surgeons and other stakeholders, began enlisting hospitals in a planned national hip-replacement registry for the U.S.)
Other countries have truly world-class registries that set the standard for international best practices, but these practices need to be replicated either at the national level or in other health conditions. For example, in 2005, the Ministry of Health in Canada’s province of Ontario established the Ontario Mental Health Reporting System , one of the few genuinely comprehensive mental-health registries in the world. But so far, the system’s coverage is limited to Ontario. A next step would be to use the Ontario system as a model and extend it to other Canadian provinces. Similarly, the success of Australia’s national hip-replacement registry needs to be replicated for other health conditions. Australia has made progress in this regard—particularly in its recent initiative to combine regional disease registries for acute myocardial infarction into the truly national Australian Cardiac Procedures Registry .
Another successful example of “going national” is the recently established National Cancer Intelligence Network (NCIN) in the U.K. Previously, the country had a number of regional cancer registries, but they were fragmented and tended to focus primarily on patient mortality. By contrast, NCIN is a truly national registry, designed to track a broad variety of diagnosis, treatment, and outcome data. The new system harmonizes and links data across the regional registries to create a patient record with consistent data. It also connects to databases outside the regional registries (for example, the cancer data set from the U.K.’s Office for National Statistics, data from a number of national clinical audits, and local-hospital episode statistics), increasing the variables available for risk adjustment. Perhaps most important, the U.K.’s national health system with unique patient identifiers allows NCIN to combine patient data for more than 90 percent of all cancer sufferers in the nation.
Moving from Data Collection to Data Use. Some countries that collect comprehensive and reliable national outcome data have yet to use their data effectively to improve clinical practices. Singapore, for example, is pursuing a major national disease-registry agenda. In 2001, the national government established the National Registry of Diseases Office (NRDO) to collect and maintain information on a set of disease conditions and to compile and publish statistics mainly for epidemiological purposes, resource planning, and setting health care policies. In 2007, Singapore passed the National Registry of Diseases Act, which creates a standardized system for the compulsory reporting of health outcome data for patients suffering from cancer, renal failure, stroke, acute myocardial infarction, and other diseases. The country also has a pioneering e-health initiative in the area of diabetes, and its introduction of “transparent” hospital billing has helped health consumers develop a clearer understanding of the costs of treatment.
The next step for Singapore, however, is to leverage this world-class data infrastructure by helping clinicians analyze the vast amounts of data being collected and to actually use the data to identify best practices and improve clinical performance. In order for this to happen, NRDO, in collaboration with professional medical organizations, will need to take a more active role in coordinating the dissemination of data to clinicians.
Reimbursing for Value. Finally, there is the rare country that already has advanced outcome-based data collection and whose engaged clinical community actively uses the data with the goal of delivering national benefits in the form of improved health outcomes. Of the countries we evaluated, only Sweden has achieved this.
Sweden has been an international pacesetter in the establishment of disease registries , some of which date back to the 1970s. Today, the country boasts nearly 90 registries covering more than 25 percent of total national-health expenditures. About one-third collect patient data on more than 90 percent of all Swedish patients diagnosed with a given condition or undergoing a particular procedure, and many have been in place long enough to provide unique longitudinal data. A recent study found that Sweden has the best health-care outcomes in Europe, even while its health-care costs, as a percentage of GDP, hover around the European average of roughly 9 percent. In September 2011, Sweden’s government declared the expansion of Sweden’s network of registries a national priority and has committed to increasing its direct financial support nearly fivefold—from $10 million to $45 million per year—by 2013.
But even Sweden has work to do. Although most major health conditions are comprehensively covered by registries, some areas such as psychiatry and primary care remain underdeveloped. There is also an opportunity to encourage national standardization through the development of a shared national IT platform.
Perhaps the most important challenge to Sweden’s efforts, however, is to engage health care providers and suppliers in developing reimbursement models that link outcome data collection, reporting, and results (that is, outcomes actually achieved) to reimbursement. At the moment, only adverse outcomes have an impact on reimbursement. But as outcome-based incentives are key to driving performance, it is important also to reward both providers and suppliers for quality improvements and to increase demand for innovation that improves care.
Although Sweden was an early mover in value-based pricing of pharmaceuticals with the establishment of its Pharmaceutical Benefit Board in 2002, Sweden’s current government has recently been discussing a plan to move away from that approach to a simpler, more cost-focused “reference pricing” model. Such a move would delay the country’s progress toward value-based health care and could perhaps even undermine its standing as a world leader. In the U.K., by contrast, the Department of Health, has recently announced its intent to introduce a system of value-based pricing for branded medicines in 2014. The new approach will create a much closer link between the price the National Health System pays for a particular medication and the value that it delivers, as assessed on the basis of improvements in health outcomes. Should we repeat our international progress assessment within the next few years, the order of the country rankings may well be different.
The Role of Government
Our work in the field of value-based health care has convinced us that although the clinical community must be at the center of each country’s efforts in value-based health care, government also has an important set of roles to play. In effect, government is a necessary orchestrator that can facilitate the transition to value-based health care.
Facilitating Engagement. In countries whose clinicians and health policy makers are not fully engaged in setting up the necessary institutions for value-based health care, government can play a facilitating role, assembling the key stakeholders and providing hands-off support for clinician groups designing, collecting, and sharing registry data among themselves. For instance, government can create incentives by providing early seed funding for registries and associated research and by providing accreditation benefits for participation. And once the “tipping point” of clinician engagement has been reached, government can also pass legislation establishing consent frameworks for the collection and use of health information, setting guidelines for registry success, and creating standards that make sure that data on health procedures and outcomes are linked to cost. Even countries at the very beginning of the journey toward value-based health care can make enormous progress by leveraging examples from around the world to demonstrate the impact of the approach.
It is critical, however, that government maintain an arm’s length distance from the process of actually defining metrics, collecting and analyzing data, and sharing best practices with clinicians. These tasks need to remain the responsibility of the clinical community itself. Overzealous actions by government—for example, glossing over valid explanations for variation in outcomes or publishing results before they are supported by the clinical community—will likely entrench resistance to change.
Building Infrastructure. Government also has a lead role to play in the creation of shared IT infrastructure and data standards, including unique patient identifiers. We are not suggesting that the government should actually run a country’s network of disease registries. The effective functioning of registries requires that the relevant clinicians have a sense of ownership and be deeply engaged in registry management. However, by encouraging—and perhaps investing in—the creation of a shared IT platform, a country’s government is contributing to the interoperability of data sets among registries and to the eventual transition to effective e-health records. What’s more, the existence of a common infrastructure will significantly reduce the start-up costs and also, therefore, barriers to entry for new registries.
Creating Incentives for Continuous Improvement. Finally, in most countries—even countries without public health-care systems—government is a major payer for health care services. It can, therefore, create incentives for the use of best practices that have been demonstrated to improve health care value. For example, government can make the collection and sharing of health outcome data a condition for reimbursement or accreditation. It can make value-based health care a priority in the allocation of the public health-care budget. And, as the existence of comprehensive health-outcome data leads to the identification of best practices, government can incorporate those practices into the standards for reimbursable treatment.
Reimbursement to pharmaceutical and medical-technology companies should also be increasingly determined by their contribution to better outcomes or to lowering the cost of care—as reflected in real-world outcome data. A health care system that is truly aligned around value will encourage and reward the development of innovative new products and services that improve outcomes and reduce costs for a given patient group.
It takes years and, perhaps, even decades for a country to make the transition to value-based health care. But the picture of what it takes to build an effective value-based health-care system is becoming clearer. And the most advanced countries are already reaping the benefits.
Acknowledgments
The research described in this publication was sponsored jointly by the Health Care and Public Sector practices of The Boston Consulting Group. The authors would like to thank their BCG colleagues Rachel Swift, who managed the project team, and Benjamin Berk, Jennifer Clawson, Karalee Close, Peter Fechner, Viktória Gerner, Bente Jorritsma, Larry Kamener, Joshua Keller, Simon Kennedy, Jan Willem Kuenen, Lydia Lilja, James O’Day, Gabriel Österdahl, Kyle Ruttan, Martin B. Silverstein, Shunsuke Tashiro, and Wouter van Leeuwen for their contributions to the research; Robert Howard for his assistance in the report’s conceptualization and writing.