The COVID-19 pandemic has massively disrupted—and exacerbated the shortcomings of—health care systems (HCSs) around the world in both the public and private sectors. But it has also served as a catalyst for needed transformation, pushing many HCSs to make significant changes far faster than they would have done in the prepandemic operating environment.
The challenge now is to build on the momentum from those efforts to deliver better care at lower overall cost and to build resilience for future waves of COVID-19—or even other potential pandemics. Public and private HCSs worldwide can do so by applying five lessons from their responses to the pandemic:
- Improve patient health outcomes by defining appropriate care for specific population segments.
- Implement new care models, realigning resources in order to rethink the way that health care is delivered.
- Apply digital solutions more widely.
- Revamp governance and policy to define shared goals and improve decision making.
- Adopt standardized data and analytics across a broader range of use cases.
Prepandemic Challenges
Even before the current crisis, many HCSs faced a variety of issues. Long-term trends, such as aging populations and more prevalent chronic diseases, have been increasing the demand for care. Costs have been rising at unsustainable rates, and patient outcomes differ widely. Many health care systems lagged in their adoption of data and analytics solutions, even as new technologies have continued to disrupt many industries.
COVID-19 compounded these challenges, but the end of the pandemic—whenever it comes—will not mean a return to the status quo. Given that projections call for health care spending to continue to grow steeply, many HCSs face increased financial pressure to bend the cost curve. What’s more, incremental changes will be insufficient. Instead, transformative change will be required, as called for by stakeholders including governments, payers, and providers.
Learning from Responses to the Crisis
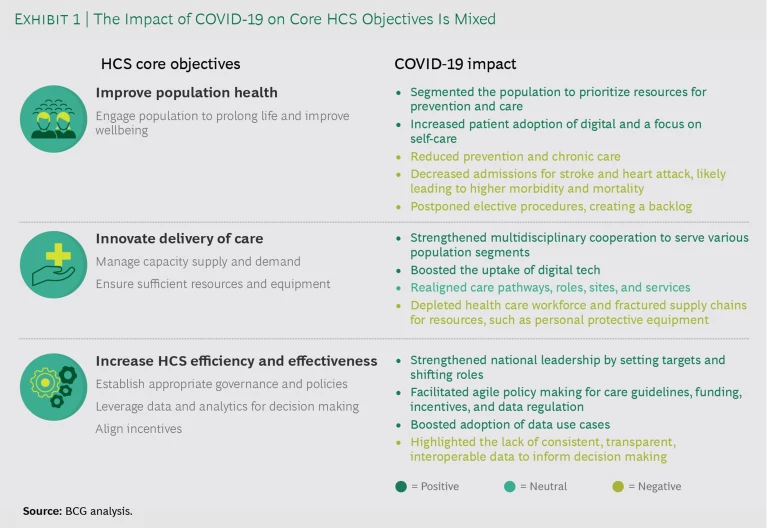
COVID-19 has had a mixed impact on HCSs’ ability to deliver on their three main objectives: improving population health, innovating in the delivery of care, and increasing their efficiency and effectiveness. (See Exhibit 1.)
Improve population health. The pandemic has served as a kind of proving ground for HCSs to implement rapid-response measures, allowing them to build up crucial experience in fast adaptation and innovation. For example, many HCSs have been able to segment the population by risk factors in order to allocate resources most effectively, such as for efforts to protect the elderly. They have also implemented telemedicine far more quickly than is typical for a noncrisis setting.
Yet the pandemic suppressed the demand for regular preventive measures, such as vaccines and screening programs, as well as routine chronic care and elective procedures. Worldwide, approximately 80 million children have missed routine vaccinations for diphtheria, measles, and polio. In Germany, the number of reported strokes has declined by 30% between mid-March and early May 2020, compared with the same period in 2019. Globally, up to 70% of elective surgery was postponed or canceled outright during the 12 weeks of peak disruption during the first wave of the pandemic, due to constraints on capacity and patient safety concerns. Delaying and cancelling procedures at this rate has a considerable impact on the health of populations, with cumulative consequences for HCSs around the world. Even if countries increased their normal surgical volume for elective procedures by 20% after the pandemic, it would take nearly a year to clear the backlog of operations.
Innovate in the delivery of care. Many countries strengthened their multidisciplinary collaboration to fight the pandemic. Spain and the US forged public-private partnerships to tap into private-sector capacity and develop new digital tools. HCSs in China and the UK created new teams with complementary clinical specialties—for example, ICU, pulmonology, and geriatrics physicians working to treat COVID-19 patients more effectively.
At the same time, overstressed care providers—challenged by both patient influxes and infections among staff members themselves—have sapped morale and depleted the workforce in some organizations. And broken supply chains for some products, such as personal protective equipment, have led to critical shortages.
Increase HCS efficiency and effectiveness. Many HCSs have shifted to more agile decision making and increased their adoption of data use cases. Sweden has been able to coordinate available beds and scarce resources by commissioning a government body to collect, analyze, and disseminate information from local health regions. And Germany created a website to collect and share information about ICU capacity at all hospitals in the country. Yet many other HCSs around the world, both national and regional, have been unable to launch similar measures due to a lack of consistent, transparent, interoperable data.
HCSs must capitalize on the lessons learned from their COVID-19 responses.
HCSs must capitalize on the lessons learned from their COVID-19 responses. In the short term, they should focus on fully implementing the innovations they have developed, such as streamlined decision making, site reconfiguration, and changes in collaborative working models. They need to take the best of what worked and build that into a new, postpandemic operating model, with the goal of delivering better patient outcomes at lower cost.
In the medium to long term, HCSs should reprioritize and accelerate transformations that were already underway before COVID-19 hit, disregarding initiatives that may no longer be relevant in a postpandemic world. To build on the lessons and insights of the pandemic, HCS leadership teams should take a hard look at the investments and plans that are in place and ongoing, and make adjustments based on what they have learned.
Last, health systems should build their organizational resilience for future crises—potentially subsequent waves of COVID-19 or another future pandemic.
Five Lessons for Health Care Systems
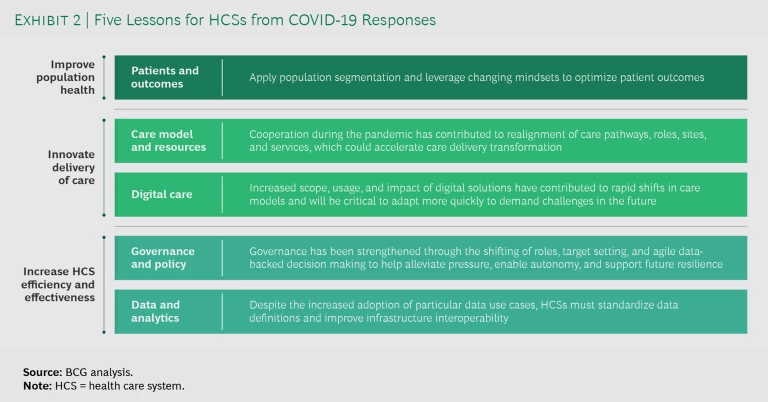
To build on their experience in responding to COVID-19, HCSs should focus on five lessons. (See Exhibit 2.)
Patients and Outcomes. First and foremost, HCSs need to focus on patients and outcomes as an overarching strategic objective that informs all other changes. When assessing the validity and value of specific changes, leadership teams should apply one metric: generating the biggest possible impact on the largest number of people at the lowest possible cost.
Other measures, such as population segmentation, are clearly valuable but require further refining. Many HCSs segmented their populations to tailor prevention and care for specific groups. But they did not apply consistent segmentation criteria across HCSs in order to facilitate comparisons and compile learnings. For example, India segmented its population by age, Sweden by risk profile, and the UK by clinical condition.
To overcome this challenge and ensure reliable, comparable clinical research results and coherent segmentation premises, an international consortium led by the World Health Organization was able to rapidly establish a consistent set of outcome measures to support COVID-19 research. And more recently, the International Consortium for Health Outcomes Measurement (ICHOM), in cooperation with more than 30 clinical experts and patients across 15 countries, developed a standard set of outcomes for COVID-19. Leveraging these standardized data definitions for patient results across HCSs will help organizations to learn more quickly and adopt best practices.
In the postpandemic environment, HCSs should build on these lessons to incorporate population segmentation when designing effective social interventions. They should also focus on preventive care and self-empowerment among patients.
Care Models and Resources. In order to combat COVID-19, HCSs have adapted the way they deliver care, implementing such best practices as cooperating through public-private partnerships, combining clinical and social care, and taking other measures to realign care pathways, roles, sites, and services. Some of those changes will have clear repercussions beyond the pandemic.
For example, the Centers for Medicare and Medicaid Services (CMS) in the US rapidly intervened to ensure that local hospitals and health systems would have the ability to handle a potential surge of COVID-19 patients by temporarily expanding capacity at care facilities and issuing regulatory waivers (also known as CMS Hospital Without Walls). CMS also facilitated increased access to telehealth for Medicare patients to ensure that they could remain safely at home and still have access to physicians and other specialists.
The UK reconfigured its care pathways during the pandemic as well, setting up COVID-19-free elective cancer hubs across London to continue delivering critical treatments and surgeries and converting nearly all outpatient interactions to virtual settings.
New workforce models have also emerged. In Australia, pharmacists have been empowered to renew prescriptions for antibiotics and medications for chronic conditions. And cross-system supply chain networks have improved procurement for entire systems. The Netherlands centralized its supply of personal protective equipment through a supply chain control tower, increasing the ability to foresee potential shortages and delays and allowing leaders to redirect needed resources to facilities with the most urgent need.
After the pandemic, HCSs need to fully implement these positive changes and apply them in non-COVID situations. For example, new care models and pathways established during the crisis can be used to treat noncommunicable diseases (NCDs). Specific care methodologies undertaken to protect the populations at the greatest risk of developing COVID-19, such as the deployment of self-empowerment digital tools for patients, could be leveraged for NCDs as well.
Digital Care. During the pandemic, the demand for digital health care technologies has rapidly grown among both patients and physicians. In some European countries, for example, patients’ willingness to use telehealth rose by up to 60 percentage points over prepandemic levels. A German insurance company increased its portfolio of digital services by more than 200% in a matter of days.
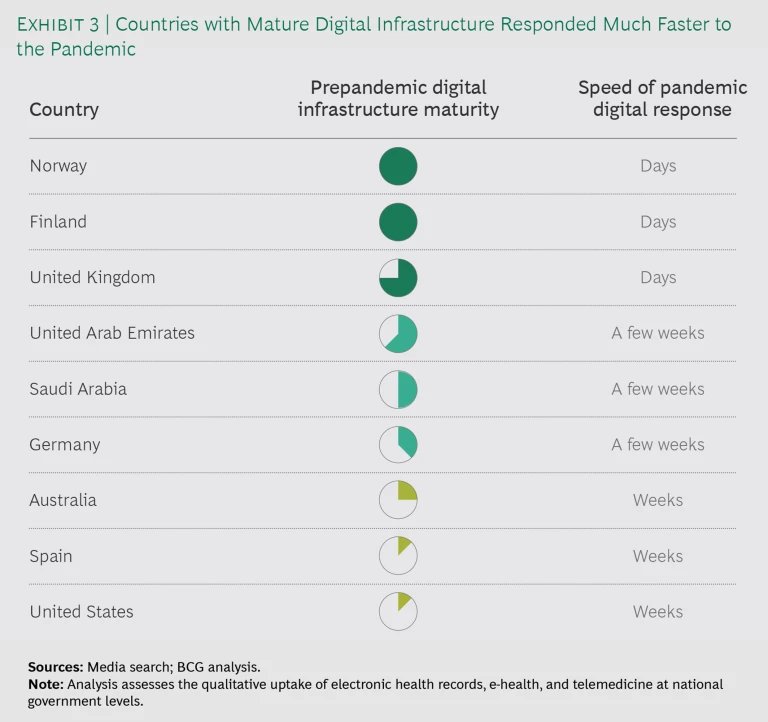
Notably, the organizations that had a stronger foundation in terms of digital technology before the pandemic hit were far better equipped to respond to it. For example, Norway and Finland both had scalable, flexible digital infrastructure in place for their national health systems, which dramatically accelerated their rollout of coronavirus response measures. (See Exhibit 3.) In Norway, the number of virtual consultations with general practitioners increased tenfold from February to March 2020.
Other health systems that may not have had such an infrastructure in place before the coronavirus have taken noteworthy steps to close the gap. For example, Dubai rolled out a telehealth app that offers free voice and video consultations around the clock. And the European Union announced a €56 million initiative in May for digital tools, including artificial intelligence.
It is unclear whether current adoption rates for digital tools, especially among patients, will remain at current levels once the immediate crisis is over. But even if they decline somewhat, they are unlikely to fall back to the levels of 2019. These new tools have already transformed care by making it more accessible and improving the patient experience at lower cost. Some estimates hold that digital solutions can increase outpatient productivity by more than 30%. Another study found that teleconsultation can reduce hospital admissions by 45%.
HCSs need to to continue investing in and enabling solutions that allow them to manage subsequent waves of the pandemic or future pandemics.
Therefore, HCSs need to continue investing in and enabling solutions that allow them to manage subsequent waves of the pandemic or future pandemics. These measures include permanently removing the regulatory and financial barriers to adoption—or at least not reinstating those barriers after the pandemic has passed. In the US, for example, 340 organizations have written to Congress to make the loosening of telehealth regulations permanent after the pandemic. More broadly, health organizations need to set clear digital strategies and investment plans to build resiliency and deliver efficiencies.
Governance and Policy. Several countries that had survived epidemics, such as SARS and MERS, had made changes to governance and decision making in light of their experiences. As a result, the HCSs in those countries have implemented contingency pandemic governance models for COVID-19 with greater agility and better coordination among stakeholders and government agencies.
For instance, after the 2015 MERS epidemic in South Korea, which has a government-run HCS, the country established an emergency operations center. The center monitors infectious diseases worldwide, responds to public health crises, distributes manpower and material resources, and conducts on-site epidemiological investigations through a multidisciplinary rapid-response team. The government’s unified response to COVID-19 led to high levels of public trust and cooperation. Transparent communications, detailed public dashboards, early interventions, proactive acquisition of personal protective equipment, and a comprehensive digital solution to track citizen movements all led to significantly lower incidences of both cases and deaths.
Some other countries that did not have such a strong foundation in place before the pandemic were nevertheless able to rapidly shift in order to support new ways of working. In the UK, bureaucratic governance, highly autonomous regional and local health agencies, and a lack of pandemic experience initially hindered the response of the country’s national health system (NHS). But it quickly adapted its governance model.
The NHS rapidly reconfigured acute-care facilities across sites and centralized leadership, designating authority to one individual in order to simplify decision making, ensure agility, and enable those closest to the patients to make key decisions. Acute-care pathways were streamlined to maximize capacity. Hospitals coordinated with community care facilities to discharge patients to less acute settings, rehab facilities, or home more quickly—but with additional visits and oversight by health care providers. Referral criteria to treat nonurgent conditions were changed to reduce unwarranted demand for acute care.
HCSs can build on that experience in revising governance and policy in the future. In particular, they should review organizational models in order to improve coordination and decision making. HCSs also need to align incentives to make sure that all relevant stakeholders make rational choices that lead to better outcomes overall.
Data and Analytics. HCSs faced a huge challenge in implementing data and analytics to inform and improve their mitigation measures. There is a clear need for clarity and standardization in such areas as interoperability, along with data infrastructure and definitions—starting with standard patient outcome definitions. For example, even now, almost a year into the pandemic, very few HCSs collect, analyze, and report cases using both age and underlying medical conditions. Such an analysis would support the development not only of measures to control the disease but also forward-looking research agendas.
HCSs that had fewer problems in terms of interoperability and infrastructure, such as those in Taiwan, were able to respond both earlier and more effectively. Other HCSs, such as the UK’s NHS, were able to accelerate research by sharing data and collaborating in order to understand the disease progression of COVID-19 and thus update treatment protocols.
Notably, the fourth and fifth areas in our analysis—governance and policy, along with data and analytics—are interrelated. Governance entails setting up data collection processes and sharing policies, and the data is then used to generate insights that inform future governance.
In addition to overcoming the ubiquitous challenges of improving data standards, interoperability, and concerns about sharing data, HCSs must take three actions to develop an effective data strategy:
- Build the right organization and infrastructure. Organizations need to break down internal silos by creating cross-functional data teams, collaborating with external partners, and developing the right governance policies for how data can be used.
- Apply a wider set of tools across a range of use cases. Rather than focusing on individual pilots with highly specific analytics tools, organizations should adopt more flexible data solutions that can be used in multiple areas and are highly interoperable with other solutions.
- Create a data-driven culture. Monitor data to drive operational improvements, with transparent impact measures at all levels of decision making. Not all of the individual data elements necessary to control a pandemic will be known early on, but HCSs with a strong data-driven culture will be better positioned to be flexible and adjust their analysis on critical patient outcome measures.
Even as HCSs worldwide continue to battle COVID-19, it’s possible to look ahead and imagine what health care could look like in the future. It may have:
- A much greater focus on prevention, with more consistent use of population segmentation.
- No more silos that separate different components of the value chain, thus enabling greater collaboration for prioritized conditions or population segments.
- An increased use of digital solutions to give patients greater control over their own care—and empower policymakers and clinical staff to make data-driven, objective decisions.
- Application of all of the above improvements to noncommunicable diseases, which account for the vast majority of health care spending, thus leading to better overall outcomes at lower costs.
By applying the five lessons we have identified, and by capitalizing on the lessons learned during their responses to COVID-19, HCSs can turn this vision into reality. To drive this transformation, HCS leaders at all levels—across stakeholders and within departments—will need to develop their organizations’ capacities and specific capabilities to enable and sustain changes to their institutions and ways of working.