The COVID-19 pandemic, racial justice movements, and concerns around the impact of climate change on global health have galvanized the public and investors to demand more concerted action on environment, social, and governance (ESG) goals from the biopharma industry. (See Exhibit 1.) While existing mandates and ESG reporting provide an initial frame for action, biopharma can address these concerns in a more proactive and integrated fashion at the product level.
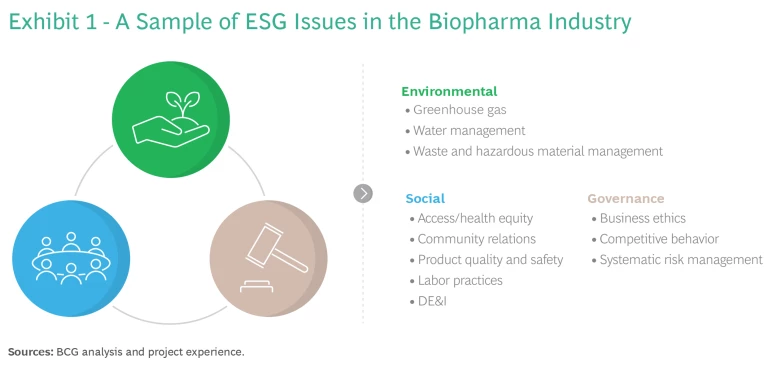
Beyond environmental considerations, biopharma’s key lever for sustainability impact lies in the social pillar—of which health equity is a core component. In the context of biopharma, health equity refers to the design and implementation of initiatives to address “avoidable, unfair, or unjust health disparities between different
Advancing health equity is not a straightforward task. Historically, biopharma has focused on global access programs and affordable pricing schemes, while also contributing to charitable endeavors. Many of these programs have struggled to be self-sustaining or failed to achieve sustained impact. While industry leaders acknowledge there is no dearth of activity in health equity, they often lament the lack of an integrated approach across initiatives and stakeholders on a meaningful scale. This has led most biopharma companies to conclude that they need to take a more systems-based approach as they design solutions to address inequities.
In this article, we propose a unified approach that addresses key challenges companies face in developing more effective health equity solutions. We believe this can be best achieved by anchoring a health equity “ethos” within existing processes—such as Integrated Evidence Planning (IEP) and Integrated Access Planning (IAP)—across the full lifecycle of all products in a systematic fashion. This effort should be linked to the overarching organizational ambition and strategy.
Various Factors Driving the Growth of ESG in Health Care
Biopharma’s need to adopt a more integrated health equity approach is driven by six industry-shaping trends:
Increased social awareness of health inequity
The pandemic exposed severe inequities in most health care systems across the world and dramatically highlighted for all stakeholders that health inequities can have a detrimental impact on individuals, health systems, and the economy.
Regulatory push for clinical trial diversity
The US Congress enacted the DEPICT Act in late 2022, which requires drug and device companies to submit a diversity action plan for FDA approval. This legislation aims to tackle the underrepresentation of racial and ethnic minorities in clinical trials. For example, while minorities make up 39.3% of the US population, a recent analysis of clinical publications showed that trials involved only 4.9% minority populations. The European Union’s ACT EU workplan, published in January 2022, similarly lays the groundwork for expanded trial diversity through mandated review boards, data disclosure in the EU-wide Clinical Trials Information System, and enabling decentralized trials to ensure a broader representation of populations.
Deploying enhanced digital and data capabilities
Health systems, payers, providers, and private industry are rapidly expanding their data and digital capabilities, which improves understanding of outcomes versus cost, helps identify outcome gaps for key populations, and facilitates information sharing. This will also give rise to new ways of generating real-world data to better understand inequities, while helping to identify and recruit patients to increase equity and diversity in trials.
Demand for more purposeful work
Employees today, particularly young professionals, want a higher level of purpose in the work they do. Biopharma companies that include ESG in their everyday fabric will have a leg up in recruiting the best talent.
Heightened investor awareness for ESG compliance and risk management
Regulatory risks for companies have increased in recent years, creating significant uncertainty for investors around the healthcare financing environment (e.g., the Inflation Reduction Act in the US) and litigation exposure due to regulatory compliance and risk management. Investors are increasingly assessing reputational and financial consequences of ESG non-compliance. Typical areas include whether companies balance pricing with ensuring patient access across countries and populations, as well as emerging opportunities related to adopting a leading ESG position in indices like the Dow Jones Sustainability Index and the Access to Medicines Index.
Push for extended health equity consideration in evaluation frameworks
Recently, health technology assessment bodies such as the Institute for Clinical and Economic Review have released frameworks to systematically integrate health equity considerations into their assessments and recommendations. As the knowledge base on methods and approaches grows, biopharma can (and must) adopt these practices in their core business.
A Roadmap to Integrating Health Equity from the Start
Leading biopharma companies are raising the bar for “what good looks like.” Examples of their efforts include:
- setting diversity goals in clinical trials
- expanding patient group engagements
- voluntary licensing and affordability programs
- health-systems strengthening initiatives
- R&D focused on neglected diseases
- charitable commitments to end tropical disease
- long-term, measurable health equity targets coupled with transparent reporting
Stay ahead with BCG insights on the health care industry
However, there is no one-size-fits-all solution for health equity. Requirements differ by disease area, geography, and population—resulting in a need for differentiated product and portfolio strategies. Integrating health equity into the lifecycle ideally begins at portfolio prioritization and early development, rather than at launch. Tackling these considerations as a go-to-market afterthought leaves much of the potential for combatting inequities untapped, while creating an unnecessary burden for market access and commercial teams.
A holistic, product-level health equity strategy begins with understanding the root causes of disparities, prioritizing research and product development based on unmet need, and engaging with the health and social ecosystems to tackle underlying drivers and deploy tailored solution sets. We’ve outlined a step-by-step guide to help biopharma stakeholders develop product-level health equity agendas by embedding the concept in existing processes.
1. Develop an organizational health equity mission and strategy as a foundation.
Addressing health disparities requires systematic, long-term action involving various internal and external stakeholders. For this reason, product-level health equity strategies developed in isolation are difficult to implement without full organizational commitment to the goal.
An overarching health equity mission should typically aspire to ensure that all patients in need can benefit from the respective treatment—independent of their place of residence, income, gender, ethnicity, or other social, environmental, or health system determinants of health. Front-running organizations include health equity as a guiding principle in their overall business strategy, with tailored initiatives depending on the portfolio.
Companies benefit from having a clear corporate mandate that embeds health equity goals and activities into the business; provides focus for the respective global, regional, and local functions; and facilitates cross-functional alignment. Industry leaders should recognize that pull-through requires expertise and capacity beyond the scope of a biopharma company, necessitating strategic partnerships and proactive engagement with governments, payers, providers, community health programs, multi-lateral bodies, and other relevant stakeholders.
When developing a health equity mission—whether stand-alone or as part of their ESG strategy— companies should ask themselves these key questions:
- What health equity concerns are relevant in the disease areas, population segments, and geographies that we are operating in?
- What are the underlying drivers of inequities?
- What is our role in developing and implementing solutions to address these drivers?
- How do we commit to health equity as we develop and commercialize new medicines?
- Who are the partners that we need to collaborate with to address health equity?
Once these core issues are identified, the following questions form the basis for articulating the health equity strategy:
- What is our ambition for health equity?
- What governance do we need? How are health equity activities coordinated?
- What is our health equity operating model? What budget and resources do we commit to health equity?
- What is our overall health equity partnership and ecosystem engagement strategy?
- How can we measure and track our progress and impact, and how is it reported?
- How is our health equity strategy embedded in our ESG strategy, integrated evidence strategy, access strategy, other product-related strategy?
Many companies have started to articulate and communicate their health equity mission. They commit to clear goals and document achievements in their annual reports. Mission and goals are cascaded through the organization and tracked through a comprehensive measurement framework, which increasingly affects incentive systems. They provide employee training programs that familiarize them with the health equity mission and their role in achieving it.
2. Prepare a comprehensive health equity framework to address the problem systemically.
Health equity concerns are highly dependent on the population, geography, and disease area in focus. The Comprehensive Health Equity Framework is a stakeholder-agnostic tool that can be applied to any health equity problem within an organization and at various scales (global, national, local). Working through and identifying the various components will give companies a comprehensive understanding of three interconnected health equity systems: determinants, solutions, and measurements. (See Exhibit 2.)
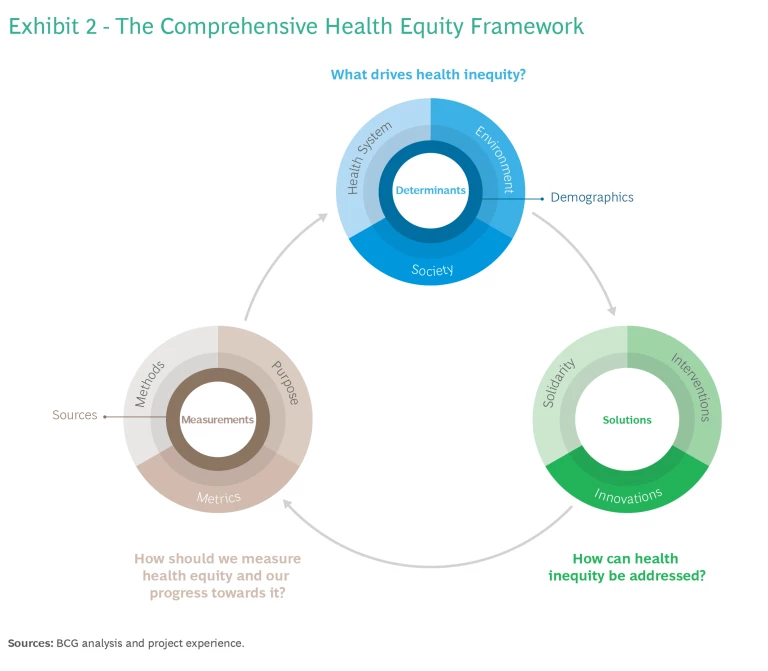
Determinants describe underlying drivers of health (in)equity that explain potential origins of avoidable, unjust, or remediable health disparities. Health equity solutions guide how disparities can be addressed. Measurements ensure understanding of both root causes and impact and that solutions are tailored and monitored effectively.
Most health system stakeholders tend to focus primarily on the health system as a determinant. However, health system-based solutions are often less sustainable and impactful because they only address disparities once they have manifested. In recent years, conversation is shifting toward the need to address social determinants of health, most recently accelerated by COVID-19 and growing awareness of racial and income inequality. Environmental determinants are increasingly recognized, given climate change and pollution concerns.
Over the full life course, these three determinant dimensions have a cumulative and compounding impact on a person’s ability to achieve good health outcomes. However, the impact of individual drivers is difficult to decouple, meaning that holistic solutions are required to address them, and that potentially different timelines to realize impact should be considered.
At the solution level, it is important first to establish solidarity, meaning behaviors that increase connectedness and align stakeholders to common goals. Then specific interventions can be identified and deployed to address individual or groups of determinants. At times, existing interventions may not be enough, such as when a new infectious disease emerges—and innovations such as vaccines, new therapies, and delivery models must be explored.
The need for purposeful and systematic measurements is often undervalued. It is critical to clarify the various measurement purposes (health impact, financial impact, effectiveness of collaborations, etc.), as no single metric can account for the full scope of interactions between systems.
The Comprehensive Health Equity Framework is intended to provide diverse stakeholders, including industry, with an overview of elements to consider when tackling this challenge. Benefits of using the tool include:
- determining the most impactful drivers and solutions
- illustrating the importance of early measurement design
- identifying individual contributions based on unique capabilities and focus areas
- encouraging early consideration of multi-sectoral implementation and governance models to ensure pull-through
Biopharma, diagnostics, and medical device companies can use the framework to launch internal conversations on strategy and activities with a common understanding and language across teams at the product-level—where equity considerations can be integrated across the full lifecycle from early development to clinical trials and commercialization.
The framework offers deep understanding of the various components of health equity and how they are interconnected. It can support development and deployment of impactful solutions over the full life course and across health and social systems at scale.
3. Integrate health equity along a product’s lifecycle
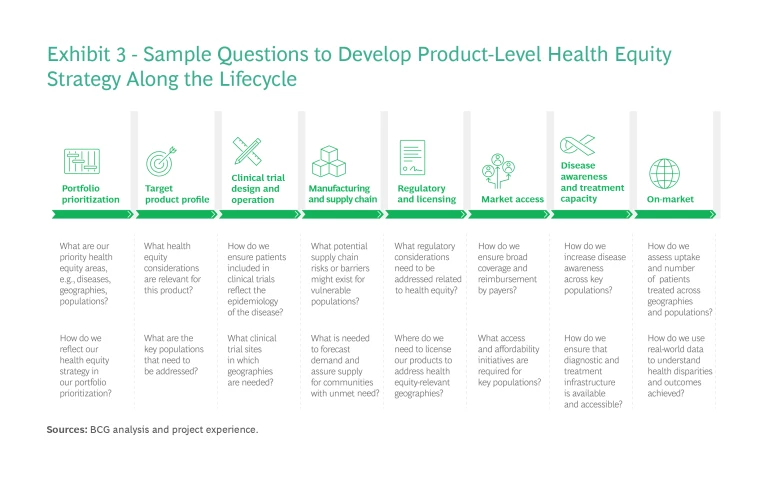
Systematic integration of health equity across the product lifecycle begins at portfolio prioritization and early development, and continues through clinical trials, manufacturing and supply chain, regulatory filing, licensing approaches, market access, demand creation and lifecycle management.
Organizations typically have established processes that guide internal stakeholders throughout the product lifecycle. We recommend anchoring health equity within the process and considering how to address and optimize it at every stage. Exhibit 3 shows a few sample questions to consider at each stage. The questions you ask—and your responses and resulting actions—should be guided by the health equity mission, strategy, and framework developed earlier.
4. Ensure pull-through and monitor progress
Once health equity initiatives have been defined, it is critical to encourage and track their implementation and performance. Organizations should strive to adopt flexible approaches to product-level equity that are continuously reviewed and refined to ensure steady progress over time, with targets laid out to account for impact that can often only be seen in the longer term. Implementing health equity plans requires specific expertise across global, regional, national, and local levels, and organizations need to be targeted in their approach towards attaining the required expertise and capabilities.
Organizations should design a robust measurement framework ahead of launching initiatives and establish a baseline against which they can track their progress, impact, and outcomes. The measurements framework should be designed with a clear understanding of the intended purpose, the measurement type (e.g., cross-sectional versus longitudinal, long-term versus short-term, descriptive versus predictive), as well as the required metrics together with the appropriate analytical methods and data sources. Metrics should be suitable to connect underlying health inequity drivers and the solutions put in place to address them.
Measurement purposes typically start at the global level and are then cascaded at portfolio/ regional level to be finally adapted to specific projects and initiatives. They can be internally focused to allow prioritization, progress monitoring, and continuous learning, or externally to report impact, outcomes, and achievements.
| Internal Purposes | External Purposes |
| • Prioritize initiatives and set goals | • Understand the local health system and levels of unmet need and disparities |
| • Ensure balanced portfolio to address unmet needs across diseases, populations, and geographies | • Access impact of initiatives and outcomes for populations and health systems |
| • Attract and optimize investments | • Build and assess the quality of collaborations and partnerships |
| • Monitor progress against plan | • Communicate achievements to external stakeholders |
| • Facilitate a learning system and create synergies between projects |
Metrics can capture progress within the organization (internal metrics) as well the impact on individuals, specific populations, communities, and health systems (external metrics).
Internal metrics can measure resources (people and budgets) and return on investments, milestone achievement against plan, and aspects of collaboration and innovation across the organization. External metrics describe equity and access across individuals and specific populations. They also track health system and social/community data and impacts. (See Exhibit 4.)
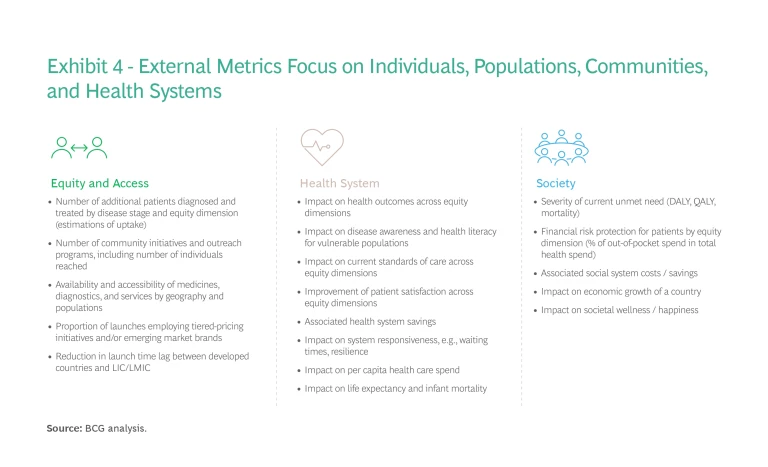
In our experience, organizations that design a clear measurement framework for their health equity initiatives are able to track and communicate their progress and the impact their initiatives have on populations and health systems. They enable continuous learning and sharing of best practices, which will be critical to expanding the scope and geographic reach of initiatives as well as attracting additional partners.
Advancing Equity Should Be a Cross-Functional, Every Day Mission
Integrating health equity into the core of the business requires bringing together different stakeholders internally and externally. While companies have control over how they consider equity in their portfolio prioritization, clinical trials design, and product manufacturing, they do have to collaborate with a wide array of external stakeholders to identify and overcome equity challenges across the care continuum. To succeed, various elements must come together across the organization and the lifecycle of a product.
Leveraging existing internal processes—such as portfolio prioritization, integrated access and evidence planning, and commercialization/launch plans—companies can embed health equity into the organization’s daily operations. Many of these processes already address equity-related considerations indirectly, but can now do so systematically and with clearer goals and measurements at a product and portfolio level. This holistic approach will help companies avoid gaps, such as late-stage go-to-market optimization for medicines that lack suitability for lower income markets, or difficulties setting differential pricing schemes that are both financially viable and affordable to meet patient needs.
Integrated health equity planning is inherently portfolio-, product-, and geography-dependent—and there is no one-size-fits-all solution. The tools we’ve outlined will help customize a systematic approach that reflects every aspect of your organization. Essentially, this process requires asking—and answering—a series of simple and interconnected questions. Identify the health equity challenges, where you are now in relation to them, and what you want to achieve. Next, develop and promote a company-wide mission, strategy, and all-in commitment to advance equity. Then map out, implement, and monitor activities across the organization and product lifecycle.
This article offers a bird’s eye view of integrated health equity planning. We are currently developing an in-depth playbook to further guide biopharma companies in this critical process. Please reach out to the authors for more information.
This content is the outcome of a longstanding collaboration between the BCG authors and Indranil Bagchi, of GSK.










