The Covid-19 pandemic delivered a generation of change in a matter of months. Digital engagement with health increased dramatically. Care teams innovated to meet the needs of patients. Among many changes, ideas and pilots were turned into full-scale virtual hospitals, electronic prescriptions were delivered at scale, a new wave of digital start-ups emerged, and, in New Zealand, clinical information systems expanded across all settings.
Despite these transformations, the health sector is still a laggard in its use of digital technology. Both patient and clinician experiences remain fragmented, and health data is under-utilised. As we emerge from the pandemic, the pace of change has slowed sharply. The potential applications of digital in health remain massive – but finding the path forward from here remains challenging.
BCG’s Digital Health in Australia and New Zealand: What’s next? describes the state of and outlook for the digital health landscape. From our partnerships across the health care value chain, and based on global expert insights and a series of interviews with regional digital health care leaders, we present a clear view of the opportunity that digital health represents. We have identified five levers for how the public and private sectors can maximise the value of digital health and continue the transformation of our health care systems.
The questions asked here are part of a broader conversation taking place across the sector: How do we make sure changes introduced during the pandemic are sustainable? How do we continue the leap to digital and enrich care for Australians and New Zealanders without a global crisis at our heels?
The Opportunity Ahead for Digital Health in Australia and New Zealand
Continuing to digitise our health system could significantly improve experiences and outcomes for patients and health care workers in Australia and New Zealand. Imagine if our health system really worked at its full potential to identify the need for care early, to secure and expand access to care, to coordinate care with and for patients, and to translate best practice to the bedside. Successful digital transformations can take these opportunities and convert them to reality:
Identify the Need for Care Early
- Predict the health needs of segments of our population before they become urgent, particularly for those most at risk such as children and the elderly
- Develop focused, proactive and preventative services rather than waiting for patients to decide when they need care or experience a health emergency
- Support individuals to understand their own risk factors and take steps to protect their own health
Secure and Expand Access to Care
- Improve the effectiveness of our workforce by using digital tools to prioritise patients and conduct passive monitoring
- Automate whatever possible to ease the burden of menial tasks on our workforce
- Improve equity and access for patients in regional areas and those with limited time, bringing the best clinical care to anyone who needs it
Coordinate Care With and for Patients
- Smooth the patient journey across our highly fragmented system by putting the patient at the centre of our planning and delivery of care
- Support patients that want to be engaged in their health care and build their digital literacy to quickly adopt and adapt to digital care
- Accelerate the transition to patient-preferred home-based care with quality and confidence, whether through hospital-in-the-home, aging-in-place, or disability support
Translate Best Practice to the Bedside
- Invest to understand the outcomes that are delivered for individuals, population segments and systemically across the health care industry
- Study variations and learn from what works clinically and operationally to democratise best practices
- Empower patients with the knowledge of likely benefits and risks of each procedure given their unique situation
- Bring together researchers, clinical trials, industry, and the care delivery network to solve the major clinical and operational issues facing our systems
- Connect real-world-evidence sources such as registries and Electronic Medical Records to understand the outcomes of products and services in real patients
“When I finished medical school, data was for me to manage my patients. Then when I joined a group practice it was our data to treat our patients, and for specialists to treat our shared patients. Now the data needs to be available to the patient for their self-management – that is our next threshold.”
—Dr Steve Hambleton, Australian Digital Health Agency Chief Clinical Adviser
“By designing a ‘digital human’ (a digital model of human physiology) we’re mapping the complex interactions between organs, from a biological, chemical and physical perspective. by building more detailed and accurate models, we can run research on virtual models rather than experiments on live organs – greatly increasing the speed of initial phase research. these models can also be individualised for precision medicine applications in diagnosis, management and therapeutics.”
—Dr Diana Siew, Auckland Bioengineering Institute, Strategic Partnerships Lead and co-chair of the Consortium for medical devices
How Will Our Digital Health System Evolve?
Based on our expertise and work with industry leaders across the public and private sectors we have identified five levers to drive success and realise emerging value in Australia and New Zealand over coming years:
- Use Digital Tools To Integrate Fragmented Delivery
- Unlock Digitally-Enabled Health Surveillance and Prevention
- Liberate the Value of Data
- Drive for Scalability and Patient Experience
- Build on Strong Relationships
1. Use Digital Tools To Integrate Fragmented Delivery
The term ‘patient journeys’ is often used to describe how people move through and interact with the health system, but for many patients the journey is anything but smooth. The problem is experienced by individuals seeking care across different geographies, providers, facilities, or professions, who often find that it feels like they are starting from scratch in every interaction. The problem is particularly acute for many of the 5 million Australians and 1 million New Zealanders living with two or more chronic conditions, who may receive a mix of disease-specific treatments that don’t consider co-morbidities.
Virtual care has the potential to overcome this fragmentation and deliver unified care to a patient where and when they need it. Virtual care includes any digital and telecommunications technology that connects physically remote patients with health care services and care teams, such as telehealth consultations. It offers proven benefits in patient satisfaction, access, convenience and cost-effectiveness compared to many forms of in-person care.
For Australians and New Zealanders living in rural and remote areas, the need to travel long distances for in-person services drives lower rates of cancer screening and higher rates of potentially preventable hospitalisations. Telehealth in rural Australia had been funded by government for over a decade, including, for example, through successful stroke telemedicine programs in some states. However, remote virtual care only reached scale as the pandemic required it to become available nationally. The dramatically increased uptake provided the catalyst for clinical practice change, technological investment and operational redesign.
In addition to overcoming access challenges, virtual care can offer a system-wide approach to improving care coordination and better meeting patient needs. It allows patients to be connected with the professionals and services most suited to them, rather than what is physically available. Virtual care conferences allow multiple health professionals across acute and primary sectors to come together and make joint decisions with patients, which is impractical for in-person meetings. Highly specialised practitioners at acute tertiary facilities can lend their expertise to patient diagnosis, management and care from the other side of the city, country or world. As models of virtual care and remote monitoring continue to grow in sophistication, virtual care can also offer patients an alternative to the revolving door of hospitals, outpatient clinics, GP rooms, and other providers.
“COVID-19 showed us what new models of care could look like. We knew the digital technologies could work, but they only made sense once we could do them at this scale.”
—Professor Mary Foley AM, former Managing Director, Telstra Health
“COVID-19 was a forcing function to do virtual care, but most didn’t do it very well… It was a survival mechanism, rather than good UX for patients or clinicians.”
—Chris Young, former Vice President of New Virtual Market Development and Incubations at Ascension
“COVID-19 was a wakeup call for the government to lift barriers to telehealth.”
—Dr Reza Jarral, NZ General Practitioner and Clinical Director of CareHQ, Clinical Director for Equity at ProCare
Where to From Here?
To deliver the full potential of integrated digital health – including virtual care – patients, practitioners and policymakers will need to establish and champion these foundational components.
Digital tools and communication need to be intuitive and easy to use for clinicians and patients. Ideally, digital health tools should use patients’ existing mobile devices. More complicated platforms should only be used when the care demands it, and ideally should have interoperable standards to avoid a second wave of fragmentation as developers and innovators compete to establish separate virtual care platforms and use-case-specific virtual care apps. The Australian Digital Health Agency’s my health app is a solid step in this direction, presenting an opportunity for further work to ensure its offering is comprehensive and broadly adoptable.
Data needs to be collected and integrated from across the system to support cross-cutting services. The health care system is not short of data or opportunities to better serve clinical staff and patients through new ways of integrating information. In addition to existing health records and activity tracking from primary to tertiary care, new forms of data include patient-reported symptom-tracking, remote monitoring and diagnostic devices. While user experience is key, virtual care will miss a bigger opportunity if it only focuses on facilitating a conversation between clinicians and patients. By integrating these other forms of data, technology can extend care – for example, devices sending prompts and reminders to patients to take medications.
Data that flows between patients and care teams needs be secure and protected, without placing a burden on small-scale providers. The Strengthening Medicare Taskforce Report has identified data and digital technologies as critical for improving primary care outcomes and supporting multi-disciplinary teams. Australia’s My Health Record and New Zealand’s Hira systems are designed to put data in the hands of patients to share with their care providers. They offer an obvious starting point for making virtual care consults efficient, effective and machine-readable for all parties.
Clinical governance and care protocols need to pave the way for ongoing virtual care at scale. It must be straightforward for care teams to work in a virtual context when this presents the patient with the best outcomes. Mechanisms that protect patients in physical settings must be extended and enhanced to protect patients in mixed modality and fully virtual care.
Virtual care needs to be rewarded by policymakers and payers with strong financial incentives. The value of improved clinical and patient outcomes, reduced overall costs, and greater collaboration between hospital specialists, community GPs, and members of multidisciplinary care teams needs to be recognised.
“We need to move beyond sharing curated data and documents, towards sharing clinical data in order to tell a fuller story.”
—Daniel McCabe, First Assistant Secretary Digital Health, Commonwealth Department of Health
All areas of Australia and New Zealand need high-speed, affordable internet to access virtual care. Large parts of both countries don’t have reliable internet access due to cost or network coverage. Models of care need to be adaptable to patients’ digital access and literacy, with the flexibility to use video-enabled care and asynchronous telehealth. The digital divide between metro, regional and remote communities needs to be closed so that health inequities do not increase as virtual care expands.
These actions will move Australia and New Zealand closer to achieving a health system that connects patients with the care and supports they need, when and where they need them.2. Unlock Digitally-Enabled Health Surveillance and Prevention
Through the pandemic, Australians and New Zealanders became experienced participants in widespread digital health surveillance, including QR code sign-ins, self-reporting of antigen test results and daily tracking of suburb-level infections and vaccinations. Core public health systems are now linked in near-real-time, with pathology results feeding directly into notifiable disease registries and vaccination evidence available on national health records within minutes. More than 65% of the Australians surveyed in BCG’s Digital Government Citizen Survey in 2022 had accessed their health records online and health records had the second highest satisfaction of any digital government service (after filing a tax return).
As digital surveillance of population health expands, so does the health care system’s ability to identify, respond to, and prevent disease transmission, moving us towards a system that is better equipped to proactively prevent disease.
Current tracking of notifiable infections in Australia and New Zealand reflects only 10% of all deaths and hospitalisations from communicable diseases.
Some non-communicable diseases, such as allergies and weather-induced asthma, could also be observed and addressed earlier by using physical tests and novel surveillance tools such as Google Search patterns or changed purchasing patterns with data privacy protections in place.
"There is a massive opportunity to expand the range of available at-home diagnostics, including for STIs, if the TGA is supportive."
—Daren McKennay, Partner, Crescent Capital Partners
“Home-based screening for flu and STIs may well be with us soon; it’s ripe for scaling because people's literacy around testing has changed enormously from COVID-19.”
—Professor Sharon Lewin, Director, Doherty Institute
Wearables and nearables (Exhibit 1) continue to increase in capability, tracking a wider range of physical, emotional and mental indicators. They are likely to become a standard tool of care, particularly for at-risk groups.
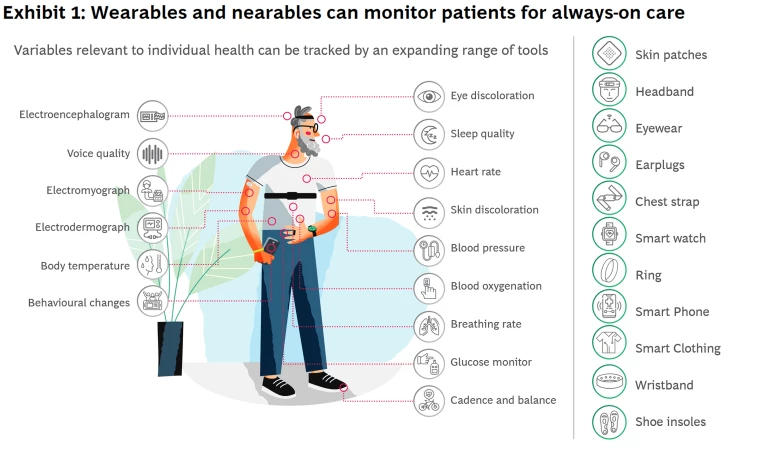
Patients will be empowered with greater visibility of their health, and care teams will be better informed. The health system is likely to move closer to continuous public health surveillance, as demonstrated by pre-symptomatic detection of COVID-19 cases using smartwatch data,
The health system can also use monitoring and surveillance to identify which segments of the population might be at risk of disease and which interventions could make the biggest difference, with more nuanced warning to support self-management. Consequently, health systems will have clearer insight into how to allocate services and resources.
At an individual patient level, predicting disease early will support the design and delivery of targeted primary and secondary preventions to slow deterioration and maintain health for longer.
Where to From Here?
Voluntary digital health surveillance needs to be on an opt-in basis and provide clear value for individuals and society. BCG’s Trust Imperative Report 3.0 found that 53% of Australians and New Zealanders are willing to share data with government to receive more personalised government services. This figure has declined from 70% in 2021. The health system needs to reflect patients’ attitudes and concerns, and industry leaders have an opportunity to build momentum for change. Regulators must neither move too slowly (jeopardising trust in system safety), nor too quickly (risking unnecessary restrictions on innovation).
"We need a radically different approach to data management. Real-time access to data in a pandemic is critically important for policy. We can’t just rely on data from other countries."
—Professor Sharon Lewin, Director, Doherty Institute
3. Liberate the Value of Data
“Australia needs national infrastructure to enable interoperability for health care. A federated health system, national infrastructure and standards are critical to glue health care together".
—Daniel McCabe, First Assistant Secretary Digital Health, Commonwealth Department of Health
The health care industry has always been data rich, and is now believed to be the fastest growing industry when it comes to data. Despite this, the industry is yet to unlock the power of this data due to fragmented systems between operations, clinical settings, and population health. These data systems are not even close to capturing the full end-to-end patient journey, which is needed to understand and implement preventative and treatment pathways.
Collecting and connecting new types of health data to existing datasets will add to the industry’s understanding of health. New types of health data are being generated from consumer devices (such as wearables), genomic sequencing, and previously inaccessible health data locked in scanned notes and images. The industry can harness the power of this data to better understand patients and their interactions within the health system.
Being trusted with health data creates cyber and digital challenges: ethics, privacy, resilience, and security. Government, technology providers, and practitioners must be able to answer these questions:
- Ethics. How do we ensure health data is used for the right reasons, and with consent?
- Privacy. How do we protect the individuals’ right to their health data, and their right to maintain its confidentiality?
- Resilience. How do we assure the veracity and availability of the data so it can be used reliably to make decisions – by humans or machines?
- Security. How to ensure responses to the above challenges are underpinned by robust data storage and protection against malicious actors?
Australia and New Zealand have solid foundations of rich national and binational registries, partially linked national data collections, and unique personal identifiers for both providers and patients. The challenge now is to translate this data into information and action using quick and safe exchanges and systematic analytics of outcomes and performance.
“COVID-19 accelerated distributed care among indigenous communities. The Māori community use of wearables to measure physiological function and activity is community-led, recognising self-determination and care.”
—Dr Diana Siew, Auckland Bioengineering Institute, Strategic Partnerships Lead and Co-chair of the Consortium for Medical Devices
“We, in health systems including the private sector, need to lay the foundation building blocks for data and digital enablement, linking it to where consumers receive care that drives equity and social justice.”
—Dr Reza Jarral, NZ General Practitioner, Clinical Director of CareHQ, Clinical Director for Equity at ProCare
Where to From Here?
Interoperability standards are needed to unlock the potential of data. Health systems can build on lessons from COVID-19 and small digital health use cases to integrate data-driven systems. We have seen this come to life across the world, such as the connected systems behind the UK Biobank, the All of Us project in the United States, and Sweden’s expansion of cancer registries to connect with other government databases. Australia and New Zealand can find more ways to treat and prevent disease and solve significant health care challenges, such as health equity for indigenous communities, understanding cancers and rare diseases, and the effects of biology, lifestyle and environment on health.
Providers will need to trust data and its applications. New applications in health such as AI diagnosis support, benchmarking of care outcomes across providers, and AI/ML validated treatment pathways will not be used by providers without first building trust through pilots.
For example, in New Zealand, Mercy Radiology sought buy-in from radiologists when introducing AI algorithms to support clinical diagnosis. Now as they move towards using predictive algorithms, Mercy has been met with high engagement and enthusiasm from their clinicians.
“At the beginning, our radiologists said, ‘You’re trying to replace me,’ but our second reader algorithms started picking up one clinically significant fracture a day, and now, when the algorithm is down for maintenance, I get texts from radiologists to turn it back on right away!”
—Dr Lloyd McCann, CEO, Mercy Radiology
The 10-20-70 rule can guide investment in digital and data. Big data is often considered solely from a technological perspective but getting the most out of health care data requires a team effort. A rule of thumb is that data investment ought to be 10% about algorithms, 20% about technology, and 70% about the business changes needed to systematically make use of the insights generated.
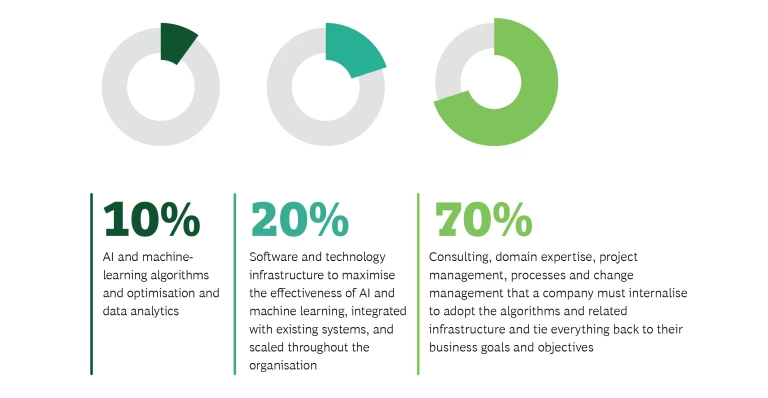
Harnessing the power and promise of big data to drive better value for patients in health care requires a collaborative approach between all stakeholders along the patient journey.
Health care organisations and governments will need to safeguard data from emerging threats. COVID-19 accelerated the rapid growth of digital health. Now, we expect a period of retrospective cyber and digital risk management as organisations consider how much their digital risk profiles have changed since the pandemic began and as they recover after the rush of technology transformations. The criticality of such security measures has only been underscored by recent large-scale violations, from Medibank to QIMR Berghofer. Expect the time for recovery to be limited by ongoing commercial cyber threats – such as ransomware or data theft – which take advantage of health data distributed in complex ecosystems. Leading organisations will prioritise defences that protect critical systems and patient outcomes, including network segmentation and segregation to minimise the impact of attacks, strict asset management to reduce unknowns in their ecosystems, and deployment of well-rehearsed response plans.4. Drive for Scalability and Patient Experience
Australia and New Zealand are attractive markets for health care innovation. In addition to a digitally literate populace, the relatively small digital health market (~1% of global market5) provides innovators with a lower-risk environment to demonstrate impact before expanding globally. Companies that are ‘born-digital’, that is, have data and digital technologies at the heart of their operating models, are those most likely to break-through to scale.
Investment in digital health in Australia and New Zealand has grown dramatically in recent years and is likely to continue. Invested capital grew at 100% CAGR to reach US $200 million from 2017–2021.6 The number of digital health deals has remained strong into 2022, even while biotech funding activity has softened sharply globally. While investors based in Australia and New Zealand are most likely to participate in the market, investment from outside the region is on the rise. International investors participated in 14% of deals in 2017, 43% in 2020, and 38% in 2021.
In one of Australia’s largest Series B funding rounds, the clinical artificial intelligence start-up Harrison.ai raised AU $129 million in December 2021, led by Hong Kong-based Horizons Ventures. Eucalyptus, a company that aims to disrupt today’s primary care and prescription journeys using asynchronous care, recently closed an AU $60 million Series C round led by US venture capital firm BOND Capital. With increasing interest from non-ANZ investors, the local industry needs to be on the front foot.
“We’re seeing plenty of trade missions shopping digital health across the US venture capital scene. It’s incredible. However, we’ve never seen an Australian or New Zealand trade mission to the US, which is a shame.”
—Chris Young, former Vice President of New Virtual Market Development and Incubations at Ascension.
Many Australian and New Zealand industry leaders are also exploring digital health start-ups. Private health insurers are looking to adopt digital health to support their members to stay well, using direct programs or partnerships with born-digital companies.
Patient expectations are high across the system. Australia’s rollout of COVID-19 anti-viral treatments highlights the many factors involved in scaling a digital prescription-to-door service that meets consumer expectations. While the technological supports are in place (e.g., risk-based triage surveys, MBS-funded telehealth from GPs, ePrescription services), the patient experience has not been smooth. It has been difficult for patients to access appointments with their usual GP and receive prescriptions to their door within the clinically recommended window. In contrast, in New Zealand, anti-viral treatments can be dispensed by pharmacists without a doctor’s prescription, which has increased uptake – especially in areas of high socioeconomic deprivation.
Where to From Here?
Patient expectations for digital services and experiences must be met. The bar for digital patient care and experience will continue to rise, lifted by digital companies that saw material gains during the pandemic (e.g., Peloton, Netflix, Amazon). Patients with low levels of health literacy or preferences for face-to-face interactions will need to be brought on the journey as well.
Providers will need to remain committed to delivering clinical value while providing increasingly sophisticated services.
Design will need to focus on patients and clinicians. Many of the patchwork, stopgap approaches to virtual care observed early in the pandemic failed. Design of digital health services needs to start with ethnographic research of patient and care team experiences, including their digital interaction and the broader processes and systems they are operating within.
“…Poor user interfaces, and a lack of true integration into clinical processes. If they can't fix these, they’re doomed to mediocrity,”
—Chris Young, Former Vice President of New Virtual Market Development and Incubations at Ascension
Direct-to-consumer digital health models with a hyper-focus on specific patient needs will continue to grow. Digital companies that cater to specific patient segments or individual moments that matter continue to emerge. Eucalyptus’ portfolio includes companies focused on fertility (Kin), menopause (Juniper), men’s health (Pilot), and sexual health (Normal). Each digital experience is tailored to the specific care need, rather than to the patient. The dynamic nature of these digital services means the platforms can adapt in real-time to what patients value.
At-home diagnostics will pave the way for new digital-first pathology services. As people experience the convenience and privacy of at-home testing, demand for new rapid diagnostics (such as rapid antigen tests for STIs and influenza) will rise if they are affordable and accessible. Companies that ‘correct and connect’ physical diagnostics into digital health care platforms – such as making pathology reports easy to read – will deliver direct benefits to patients.
"Health is about the patient, not the provider – we seem to have forgotten that along the way."
—Dr Steve Hambleton, Director Digital Health CRC and Chief Clinical Adviser to ADHA
5. Build on Strong Relationships
COVID-19 saw everyone working together in new ways to keep communities safe.
The pandemic placed massive demands on the health care industry and, for the most part, the industry delivered. As part of the push to innovate, critical health care relationships were strengthened and will become the backbone of a more digitally enabled health system.
Relationships between patients and care teams. Patient relationships with primary care teams have always been important. 91% of Australians and 94% of New Zealanders have a usual GP who became the first point-of-contact for care and support during COVID-19, as the acute system was in crisis.
Relationships within an organisation. Sharing information within organisations reached new levels. Within hospital groups, monitoring was essential to assess risks to public health, financial position and workforce strains. Hospitals needed to understand exactly how the network was performing, from available beds and ventilators to the epidemiological trends of who was most sick and who was at most risk of transmission. Organisations took an agile approach to build these connections.
“During the pandemic, everyone (health care providers, governments and software vendors) came together to deliver digital capabilities at pace and scale. We need to leverage these partnerships and deliver more connected capabilities to support health care.”
—Daniel McCabe, First Assistant Secretary Digital Health, Commonwealth Department of Health
“At times in the past, the health system was designing our approaches around the technology, rather than shaping the development of the technologies for what we need in our health care systems.”
—Dr Jean-Frederic Levesque, Chief Executive Officer, NSW Agency for Clinical Innovation and Adjunct Professor at the Centre for Primary Health Care and Equity at UNSW
Relationships between organisations. Co-operation across the system also reached new levels, with rapid connectivity to make COVID-19 test results, vaccination history and health records available immediately. Partners from across the system – including pharmacies, public hospitals, the Ministry of Health, Aboriginal Community Controlled Health Organisations, pathology centres and GPs – were connected by a digital infrastructure that also made it easier to deliver other digital services, such as a fully digital patient journey from consultation to electronic prescription to medication delivered to the door. Technology also did more than support the provision of care – it opened new doors as therapeutics and vaccines were scaled in months rather than years.
Where to From Here?
While the health care ecosystem has recognised the transformational impact of these relationships and is continuing to strengthen them, some specific actions are needed to see them thrive.
Business, government, and social entrepreneurial efforts will need to align. Active and authentic engagement across sectors will realise ambitions and clarify the strategic investments and policy settings needed to support the transition to digital health. Focusing on the lessons learned by global peers will also make it easier to avoid mistakes.
The health care system will need to look beyond organisational silos. To collectively improve patient experience, all parts of the system will need to make progress so that one weak link doesn’t break the digital chain. This includes a digital front-door approach, taking up the mindset that part of the industry’s role in supporting health is to seamlessly steer patients to the care that makes sense for them.
“Working together (Federal government, the states, community sector and private industry) means we’re more likely to come up with building blocks that can be reused and repurposed across the system.”
—Professor Mary Foley AM
The health workforce will need to be engaged and trained in digital throughout their careers. Digital will become the easier and more intuitive way to connect across the system. Clinicians will choose to use digital channels to connect with other care providers, researchers and clinical trial operators. This means the health workforce will need to be equipped with knowledge and capability to use digital tools.
Policy will need to keep pace with and to adapt to disruptions. Policy will need to be more flexibly applied and adjusted – including regulation, health technology assessments, and funding. Real-world evidence can support post-market reviews of products, services and software, and support the ongoing assessment of digital health solutions.
A digitally enabled health care system has huge value for government, industry and patients. Not only can digital health be used safely, but patients value it – particularly those who need it the most. Making the most of the changes the pandemic made possible can change the trajectory of care for the most vulnerable, while reducing the cost to the system.
Telehealth now represents ~40% of all chronic disease MBS consultations, and ~50% of all mental health consultations
To achieve the next frontier of digital health in Australia and New Zealand, the health care system will need to:
- Integrate the predictive power we have for individuals and population health to develop proactive and preventative services
- Work hand-in-hand with care teams to design what works for them and their patients
- Plan for the patient and their health care experience, smoothing out the fragmented silos of our system
- Drive change across the health care industry to make progress together, uniting around a new vision of digital health
“Now is a great opportunity to change, because the public understands its value”
—Professor Sharon Lewin, Director, Doherty Institute
As we share our predictions for the digital health market in Australia and New Zealand, we look forward to collaborating across the industry to realise the potential of digital health.











