Basic AI is becoming table stakes in health care, and leading hospitals and health systems are taking advantage of the latest iteration—generative AI—to improve performance, reduce costs, and provide a better experience for patients and staff. (See “What Is Generative AI?”) Some organizations are just starting to experiment with initial use cases and are focusing primarily on administrative functions, while others have 100-plus use cases in place, including clinical applications at scale.
What Is Generative AI?
GenAI can:
- Identify and classify content. Gather, organize, and validate existing data, such as sorting through patient information to identify clinical-trial candidates.
- Manipulate and translate content. Edit, update, and convert information, such as automating prior-authorization documents for medical procedures or translating records of previous treatments, signs, and symptoms into a new format.
- Summarize content. Create summaries and synopses of existing content, such as conversations between patients and providers for clinicians to review for EMR documentation.
- Support clinicians and administrators. Leverage the three applications above to analyze and generate text or images to supplement the work of clinicians. GenAI could be used to analyze images and EMR notes in order to detect early signs of infection in a ventilated patient or expedite annual wellness visits by identifying key details in a large patient record.
GenAI cannot:
- Go beyond the data. Solutions cannot incorporate input beyond the underlying data to reach conclusions in the way that a radiologist can incorporate such factors as pathology, undocumented patient history, and complex genetics into a clinical decision.
- Think critically and empathetically. GenAI applications do not have the ability to execute tasks involving critical or creative thinking, emotional understanding, ethical decision making, real-world experiential knowledge, or interpersonal relationships in the way that clinicians do in working with patients.
- Replace the role of clinicians. Although it can perform some tasks better than people, GenAI has limits and is not flawless. Clinical applications will therefore continue to require a clinician’s review. The technology does not replace the clinician’s role—it enhances it.
There’s no benefit to waiting to apply GenAI. In fact, leading organizations can capture an advantage by accelerating their adoption of the technology. But that’s a significant challenge, given that less than 30% of digital leaders in the health care industry feel prepared to adopt AI , and given that GenAI is evolving faster than most complex health care organizations are designed to adapt.
Implementing the technology does not need to be overwhelming, however. Based on our experience working with leading providers, we have developed a simple, five-step approach that helps leaders systematically apply GenAI. It allows organizations to identify the most powerful applications for their unique needs, begin capturing value, and build the internal capabilities needed to manage risk and generate greater value in the future.
1. Identify a Compelling Portfolio of Problems Across the Organization
Like any new technology, GenAI is sometimes treated as a solution in search of a problem. That’s a recipe for failure. Instead, organizations can start by identifying key unmet needs or challenges that the technology is suited to address.
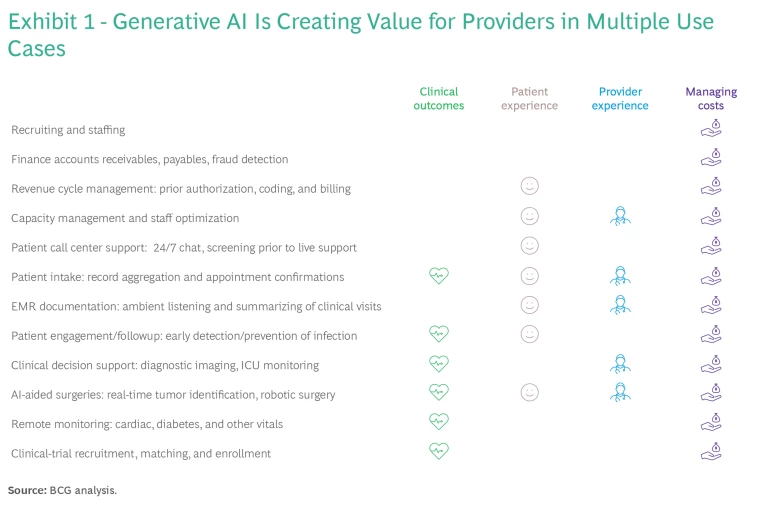
Exhibit 1 shows some of the more than 1,000 GenAI applications that can lead to better performance in the following four main areas:
- Improving Clinical Outcomes. AI-powered support tools enable clinicians to make more-informed decisions. For example, they can automatically review diagnostic images and flag anomalies, allowing clinicians to prioritize those that indicate the greatest potential risk to patients.
- Improving the Patient Experience. GenAI-powered chatbots can explain the details of a treatment plan—in the patient’s native language and factoring in literacy level—leading to better adherence and easing the burden on clinical teams.
- Improving the Provider Experience. Scribing solutions can record and transcribe patient-provider conversations and provide summaries for clinicians to review and approve for EMR documentation. This helps reduce the amount of time that clinicians spend on EMR processes—up to 40% of their day—and also helps reduce burnout in a talent-constrained market.
- Managing Costs. Administrative revenue cycle management (RCM) processes can be automated and streamlined. Documentation such as patient referrals, prior authorizations, and medical coding can be autopopulated, increasing the efficiency and accuracy of submissions and augmenting the capacity of the workforce. Thoughtful AI coding and note review can reduce claims denials by 15% and the time spent capturing charges by 80%. (See “How Generative AI Improves RCM Functions.”)
2. Manage Change
Technology is advancing faster than most health systems are designed to respond—in part because new solutions often entail changes to workflows and processes. But the COVID pandemic showed that rapid change is possible, with health care organizations adopting technology to support the shift to remote work and telehealth, for example.
Implementing GenAI follows the 10-20-70 formula : algorithms require about 10% of the effort, data and technology another 20%, and the remaining 70% goes to change management such as transforming operational processes and clinical workflows.
Our experience suggests that physicians and nurses are reluctant to adopt new technologies until they pass a high threshold of trust and reliability. When implementing GenAI, organizations can support staff by articulating a compelling vision, generating early proof points in small pilots, and including clinicians and staff throughout the process. With the right approach, technology can help an organization streamline a complex web of workflows. However, leaders need to support the effort with strong change management to ensure that staff feels heard and supported throughout the transition.
3. Think Through the Policy and Risk Mitigation Aspects
In caring for patients, providers are understandably concerned about risk. Organizations need to understand the risks that GenAI might entail—as well as the risks it can reduce—and build guardrails into the design of the new solutions.
Some health systems may not have the institutional expertise to understand how GenAI fits with their existing policy frameworks. The goal is not to formalize all policy implications in advance. Rather, organizations can start with a clear understanding of their current policy principles and then adapt them over time to incorporate GenAI across five broad areas:
- The Overarching Approach. Define the ethical principles that apply to GenAI product design and implementation. For example, an organization could align its approach with the concept of “first, do no harm,” meaning that a clinician will always make the final call on any clinical decision.
- Principles, Policy, and Training. Over time, formalize principles into policies and training programs. Providers do not need to start from scratch but can apply the experience of other organizations. For example, they can tap the existing (and evolving) policies and guidelines of professional organizations, payers, and regulatory organizations such as the American Medical Association, the Radiology Society of North America, the US Centers for Medicare and Medicaid Services, and the US Food and Drug Administration.
- Governance. Leverage existing governance, risk taxonomy, and risk management practices relating to digital solutions and data (such as the protection of patient confidentiality) and adapt them to GenAI.
- Monitoring. Ensure that GenAI solutions align with established boundaries, policies, and evolving compliance and regulatory requirements. This begins with ensuring that you identify the applications that use the technology across the organization. Policies may vary for different applications; for example, a solution that uses patient data internally will require different controls than one that involves sharing patient data with a third party.
- Responsibility Culture. Build a cohesive, value-based community focused on reinforcing GenAI policies, such as putting patients first or ensuring equitable access. The principles of responsible AI can help organizations create a culture with the right underlying principles.
Providers will need to commit to ongoing review processes as new GenAI applications and solutions emerge. For example, they can expect to reassess their policy and risk mitigation practices every 6 to 12 months.
4. Prioritize Use Cases by Potential Value and Ease of Execution
In prioritizing use cases, it’s helpful to segment across two dimensions: potential value and ease of execution. (See Exhibit 2.) Often it’s not possible to quantify the full value of an initiative, including new revenue, cost management, and patient value. But organizations can simplify the process and make various options broadly comparable by using a basic, five-point scoring system, with five indicating the greatest potential value and one reflecting the least.
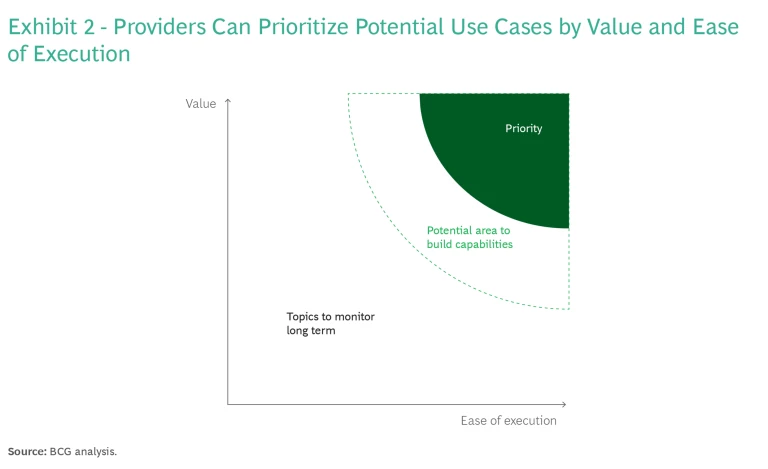
Regarding ease of execution, it’s helpful to understand the organization’s ability to implement a GenAI application and sustain it over time; that means determining whether the necessary people, platform, and partnerships are in place. Key questions relating to each of these include:
- People. Do we have the right talent, organizational structure, and operating model to support GenAI? Who are the champions? Do we have the right organizational structures in place, such as digital accelerators or incubators?
- Platform. Is data accessible, at sufficient levels of accuracy and interoperability? Which tools, systems, and vendors are we going to use? Are new solutions designed to ensure security and compliance? For example, many large hospitals have migrated to standard EMR solutions, such as those of Epic or Cerner, which have begun rolling out foundational GenAI solutions with integrated partners to ease the initial launch burden. Those on multiple EMR systems can still leverage emerging GenAI applications through a common patient interface for activities like scheduling and payments.
- Partnerships. What partnerships and outsourcing strategies are currently available? Will we co-create with partners, customize existing solutions, or adopt plug-and-play solutions? For example, a hospital specializing in complex cancer care could build GenAI solutions in cancer diagnostics, but it could buy off-the-shelf options for making administrative processes more efficient. In contrast, an integrated delivery network with a wide network of facilities could build its own network capacity management solution.
After weighing these considerations, providers can assign basic clothing sizes—S, M, L, or XL—to the ease of execution of each use case to determine the overall scope of the project. They can then select a portfolio of projects, including some quick wins that are relatively simple to implement and can generate value in a year or less, along with more ambitious and complex efforts that have greater potential impact over the long term.
Our experience shows that quick wins often focus on administrative support functions—areas characterized by high-volume, repetitive processes such as payments or appointment confirmations. In contrast, broad clinical decision support applications have greater potential value but are generally more complex. As with other digital solutions in health care, initial clinical GenAI offerings typically focus on narrow, disease-specific use cases, such as monitoring type 1 diabetes. Over time, the number of applications will grow to support a wider range of clinical decisions.
5. Track Key Metrics
The forgotten step in many health care transformations is tracking progress and improving over time. The beauty of digitizing processes is that it simplifies the process of tracking and reporting key metrics. Optimally, each problem that the organization identifies—and the corresponding solutions—are linked to a a quantifiable goal, such as reducing costs in a specific process or function by 20% or increasing patient volume by 5% to 10%.
Generative AI has immense potential to transform hospitals and health systems. By applying the five-step process outlined here, providers can reduce costs, improve the patient and provider experience, and generate better clinical outcomes. GenAI will not replace the role of clinicians, but organizations that fail to leverage the technology will be overtaken by those that do. Do you have a portfolio of problems across your organization? As a leader, do you feel ready to leverage GenAI? Is your organization ready?
The authors thank Kazim Zaidi, Stephen Filler, Keith Fairbank, and Aryana Jacobs for their contributions to this publication.

















