The UK faces several challenges over the coming years as we exit a period of almost unprecedented uncertainty. But there are two that stand out – the poor outlook for the economy and the huge pressure weighing on the healthcare system.
The country’s low productivity, falling real wages and lagging business investment are hitting the
economic growth
outlook while inflation and interest rates are rising sharply – precipitating a cost-of-living crisis. At the same time, both NHS waiting lists and the number of people out of the workforce due to long-term illness are at record highs of 7.42 million
Neither of these challenges are insurmountable. But solving them needs creative thinking and urgent action.
With its vast amount of healthcare data and leading position in life sciences and artificial intelligence (AI), the UK has a unique opportunity to unlock the value of this resource and work towards becoming a healthier and wealthier country. Capturing the full benefits of healthcare data – an opportunity that has been long mooted but never grasped – can lead to better patient outcomes, more efficient healthcare delivery and will help drive R&D, innovation and investment across the life sciences and tech industries. Where healthcare data has been used in this way, both regionally in the UK and in other countries, there have been significant benefits realised. In this paper we discuss the current challenges in utilising healthcare data and outline 18 key recommendations for policymakers to unlock the value of healthcare data in the UK. The full recommendation list can be found in Chapter 4 of the paper.
Click here to read the full report or continue below for the executive summary and recommendations.
Examples of impact from healthcare data use
Examples of impact from healthcare data use
To understand public perceptions around access and use of healthcare data, BCG conducted a representative survey of the public in England (references to the NHS in this report refer to NHS England but much of our analysis is relevant across all nations in the UK). Our survey found that, contrary to popular belief, people are generally open to allowing access to their healthcare data. However, the public’s support for data sharing is dependent on targeting the most impactful use cases, articulating outcomes and ensuring that security and privacy concerns are addressed.
Recommendation: Detail the outcomes from specific use cases of making healthcare data more accessible to generate public support and understanding.
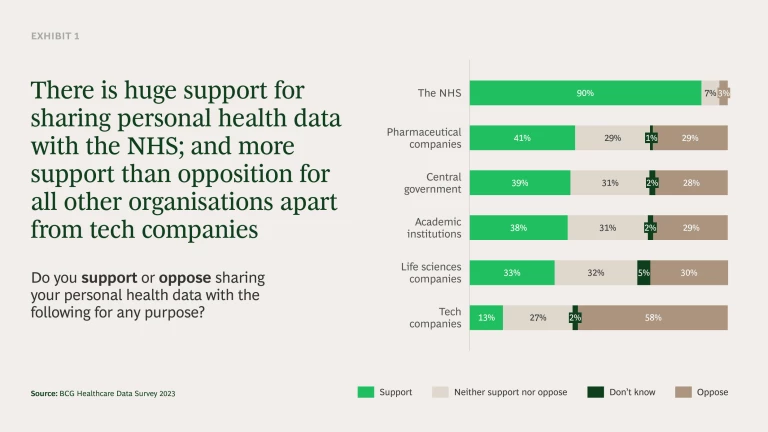
Support for sharing data with the NHS is very high, with 90% of people willing to share data with the NHS for any purpose. While support is lower for other organisations, there is still much more support than opposition – with the exception of tech companies (see Exhibit 1). Here, building public trust will be vital if they are to be involved in this space.
Our report and survey demonstrate that when the potential benefits are clearly communicated and the right processes are put in place to manage trust, the public are supportive of allowing access to their data. However, previous missteps mean trust is fragile and cannot be taken for granted or squandered. Much work is already under way, building on the Goldacre Review and the NHS’s “Data Saves Lives” strategy . But it is important the UK does not miss the opportunity to progress efforts in a way that maximises the potential value, both in terms of patient outcomes and wider economic benefits. We have identified and tested public support for a series of actions that can help achieve this dual value proposition.
The move from data sharing, where data is transferred to external parties, to data access, where data is hosted on platforms known as Secure Data Environments (SDEs) and access is controlled, has been under-discussed with the public. Our survey shows that when people are engaged on this point, a substantial majority (86%) said they felt more comfortable with data access over data sharing. The UK is therefore already starting from a stronger position than ever before.
To build on this we believe it is crucial to move towards targeting specific outcome-based use cases. These will help build and maintain public support and, by properly targeting the use cases and designing the SDEs with them in mind, the potential value of data can be maximised. Leveraging AI and machine learning is a common theme which will be crucial across the piece if these outcome-based use cases are to be achieved. For example, modelling of early AI R&D technologies has already indicated a potential reduction in time and cost of drug discovery by a minimum of 25-50%.
Recommendation: Focus on outcome-based use cases in the following four areas:
- Prevention
Recommendation: Allow for integration of a wider variety of non-healthcare data into the SDEs including socioeconomic and demographic data from tax records, welfare claims and census records, behavioural information from consumer data and lifestyle data from wearables and mobile phones. This will support better identification of at-risk groups within the population, helping to prevent disease before it develops or worsens. It will also help to improve communication, ensuring better targeting so people are more informed about their risks and healthier life choices. - Disease pathways
Recommendation: Fully integrate the widest range of healthcare data into SDEs, including biomarkers and multimodal health data. This will help maximise understanding of diseases including better mapping of how diseases spread and develop, and the biomarkers used to identify them. It will also allow for more personalised interventions, as it increases the knowledge of how different groups respond to different treatments. - Clinical trials
Recommendation: Improve the process of setting up and recruiting for clinical trials in the UK by developing an accessible ‘concierge service’ to quickly determine whether a particular trial is feasible, as well as tools to explore the sensitivity of inclusion/exclusion criteria for clinical trial participants. Along with other steps such as those set out in the recent Lord O’Shaughnessy review , this can help restore the UK’s position as a leading place to conduct clinical trials. In turn, this should help drive investment and innovation into the UK across related sectors and ensure the UK is at the forefront of healthcare discovery. - Clinical care
Recommendation: Leverage new technologies including machine learning, generative AI and AI-driven algorithms to optimise clinical care decision-making and resource management in the NHS. This can help improve diagnosis in hospitals, potentially reducing waiting times and improving treatment by giving a richer view of the impact of past treatments on different patients.
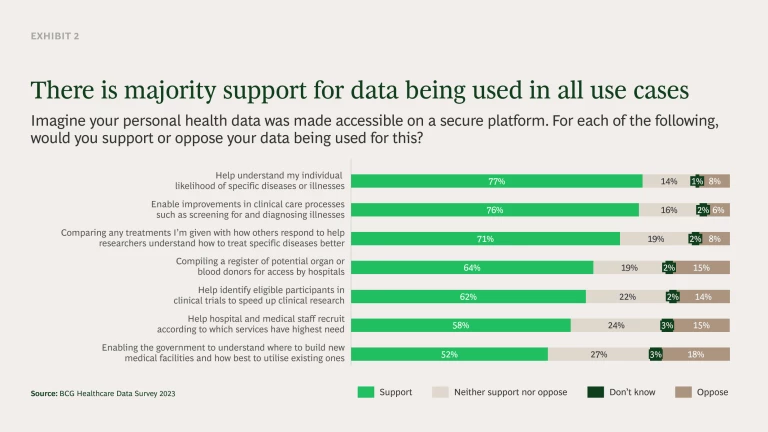
We tested these use cases with the public in our survey and found broad support for all of them (see Exhibit 2). This illustrates that when the potential benefits and outcomes of accessing personal health data are properly explained, people are supportive.
As well as targeting these outcome-based use cases there are several success factors that are crucial for realising the full potential of data and the creation of the SDEs:
Data transparency and public engagement
Trust and transparency are prerequisites when it comes to healthcare data. It is vital to proactively build public trust and ensure transparency at every stage of data access. This includes a genuine willingness to understand and communicate lessons that have been learnt from past mistakes.
Recommendation: Put in place the right frameworks and mechanisms to deliver the level of transparency and information needed, including a clear effort to be open about what lessons have been learnt and how processes have been adapted. This will ensure that public trust is maintained over time.
In the short term, a key part of this will be establishing better public communications around healthcare data usage and its potential benefits. This should form part of a wider long-term public engagement strategy that is coherent across NHS data projects. A common misconception has been that individuals oppose access to their personal health data by default, which has led to a general unwillingness to engage the public on the topic. However, our results show that nearly three quarters of people (73%) either wanted to be proactively told about the use of their data (37%) or be able to request the information (36%) when they wanted. It is therefore important that stakeholders do not shy away from conversations about how, where and why data is accessed. Section 3.1 of the report details the key areas this campaign must address based on our survey findings.
Recommendation: Establish a joined-up public engagement strategy that is consistently adopted across all NHS data projects with a specific communications campaign around healthcare data usage and the potential benefits.
In the longer term, the NHS should establish public decision panels, such as the public participation panel already used by Genomics England, and more accessible data usage registers for engaging the public in decisions around how their data will be accessed and used. Our survey showed 42% said the use of public decision panels made them more comfortable with data being collected and accessed, while 47% were reassured by data usage registers. These steps are key to ensuring the public are empowered with the right information and proactively involved in the decision-making process.
Recommendation: Use public decision panels and data usage registers to engage the public in decisions around how their data will be accessed and used. This will help ensure they have a say in decision-making processes and can review and refresh these processes over time (e.g. assess what level of engagement is needed from participants with relevant characteristics).
Use of COPI notices
During the pandemic, Control of Patient Information (COPI) notices were used to expedite the gathering of and access to data across the healthcare system, even if individuals had opted out of data sharing. COPI notices were used to support understanding of disease and were critical to the UK’s rapid identification and delivery of treatments, including vaccines.
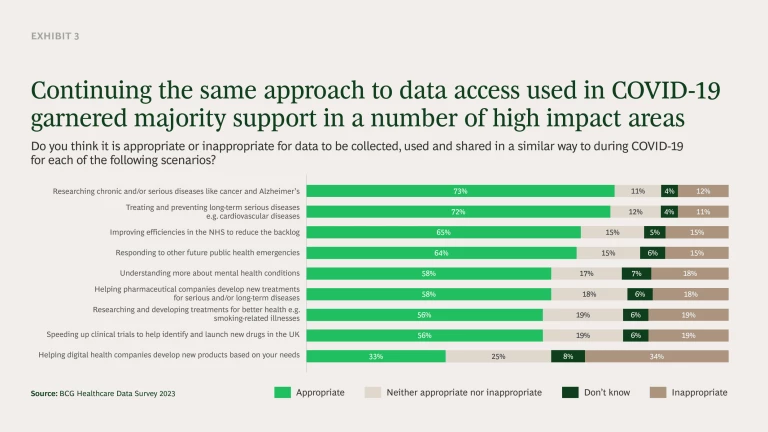
We found there is broad support (53%) for deploying a similar approach in the future. This rises significantly if used to address some of the most acute challenges facing the NHS (see Exhibit 3). Nearly three-quarters of respondents support the use of notices (or similar) for researching chronic and/or serious diseases (73%) and treating and preventing long-term serious disease (72%). Two-thirds (65%) also supported the use of these regulations to improve efficiencies in the NHS that would reduce patient backlog. Consideration should be given to using this approach for the most difficult challenges facing the NHS in the future. However, it must be done in such a way that engages the public early, involves them over time and clearly explains the benefits and end goal.
Recommendation: Consider using COPI notices more frequently beyond COVID-19. This includes utilising them for researching chronic and/or serious diseases, treating and preventing long-term serious diseases, and improving efficiencies in the NHS to reduce the backlog, as supported by the public.
Design and operation of SDEs
As part of the shift from data sharing to data access, the government is building a series of SDEs at both a national and sub-national level to bring together data for research. Section 3.2 of the paper includes more detail on our series of recommendations to ensure they are set up in a way that maximises patient and economic benefits. The common theme is that the SDEs need to be fully resourced over the medium and long term – a potentially costly exercise. It is therefore vital that their value is fully captured and partially reinvested to cover their running costs and development over time. It will also be essential to have sufficient support from the Integrated Care Boards (ICBs) to ensure that the SDEs are sufficiently funded and resourced.
Recommendations:
- Review the Data Access Request Service (DARS) process once the SDEs are fully up and running to ensure it is as streamlined as possible whilst maintaining the vital security and ethical checks on those seeking to access the data. Ensure the DARS process is sufficiently resourced.
- Review and revise (where appropriate) the necessary purpose and benefits of data access to also capture wider potential benefits to the UK economy from innovation.
- Create a service wrapper that provides all NHS SDEs (national and sub-national) with the same basic governance and administrative processes. For example applications for permissions, requirements for approval and management of the users accessing the data.
- Maintain an element of competition between SDEs – such as on services and analytical tools, including marketplaces for them – to help foster innovation and drive improvements.
- Integrate data across the national SDE and sub-national SDEs, as well as the Federated Data Platform which is also being built.
- Bring skills into the NHS to ensure the quality of data on the SDEs is of the necessary level and the workforce are equipped to analyse the data and use the analytical tools provided.
- Ensure sufficient funding is put in place to target outcome-based use cases.
- Introduce targets to hold ICBs directly accountable for creating research opportunities to ensure sufficient resourcing of SDEs.
Capturing value from data
The NHS must capture and reinvest the value created from data access. This is vital for ensuring the effectiveness and longevity of SDEs and realising the wide-reaching benefits of better healthcare data access.
A simple way to do this would be to charge certain organisations for access to the SDEs, though this may risk missing some of the value created down the line. Furthermore, the current approach taken by the NHS is to make access to the SDEs free. If data access is to be free, it is vital the NHS uses alternative value-sharing mechanisms to adequately capture the potential value. This may require a flexible approach that draws upon a range of short- and long-term value-capturing mechanisms, depending on the situation. Clear guidance should be provided so all parts of the NHS are consistently able to understand the potential value in data use and negotiate appropriate terms that deliver maximum value. Some of this must then be reinvested back into local NHS services.
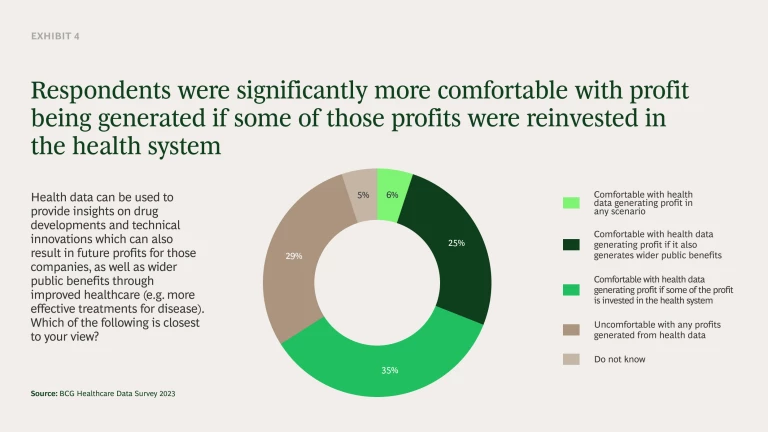
This final point is crucial. We found that 66% of the public do not mind value or profits being generated from their healthcare data providing some of that value is reinvested into the health system and/or there are wider public benefits (see Exhibit 4). When this happens, the level of support for profit-making from health data was more than double that of those uncomfortable with any profit-making. We believe the best way to reinvest into the healthcare system would be to create a central fund where revenue from healthcare data is collected and used to reinvest in local NHS services as well as to help resource the SDEs over time.
Recommendations:
- Establish a range of value-sharing mechanisms to ensure the NHS captures maximum direct (e.g. financial) and indirect (e.g. health benefits) value from providing access to healthcare data.
- Provide guidance for negotiating with commercial partners on how best to leverage the full range of value-sharing mechanisms. This will ensure maximum value according to the characteristics of each situation, including long term value via intellectual property (where appropriate).
- Ensure value acquired through data is reinvested into local health systems and the SDEs.
There are few policies that could address pressure on the NHS and boost our economy – making better use of healthcare data is one. Furthermore, it does not need major additional investment or spending. It is an opportunity the UK cannot afford to miss.
About Us
BCG's Centre for Growth brings together ideas, people and action to drive the UK forward. We work with our global expert network to identify transformational opportunities, connect key decision-makers and build coalitions for change. We offer long term strategic insight, extensive cross-sector expertise, platforms for dialogue and bias to action.














